 | |
| Clinical data | |
|---|---|
| Trade names | Kengreal, Kengrexal |
| Other names | AR-C69931MX |
| AHFS/Drugs.com | Monograph |
| License data | |
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 100% (IV) |
| Protein binding | ~97–98%. |
| Metabolism | Rapid deactivation in the circulation (independent of CYP system) |
| Elimination half-life | ~3–6 minutes |
| Excretion | Kidney (58%), Bile duct (35%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
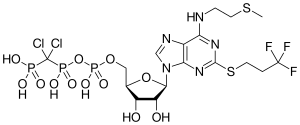
| Formula | C17H25Cl2F3N5O12P3S2 |
| Molar mass | 776.35 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Cangrelor, sold under the brand name Kengreal among others, is a P2Y12 inhibitor FDA approved as of June 2015 as an antiplatelet drug[5] for intravenous application. Some P2Y12 inhibitors are used clinically as effective inhibitors of adenosine diphosphate-mediated platelet activation and aggregation.[5] Unlike clopidogrel (Plavix), which is a prodrug, cangrelor is an active drug not requiring metabolic conversion.
Poor interim results led to the abandonment of the two CHAMPION clinical trials in mid-2009.[6] The BRIDGE study, for short term use prior to surgery, continues.[7] The CHAMPION PHOENIX trial was a randomized study of over 11,000 patients published in 2013. It found usefulness of cangrelor in patients getting cardiac stents. Compared with clopidogrel given around the time of stenting, intravenous ADP-receptor blockade with cangrelor significantly reduced the rate of stent thrombosis and myocardial infarction.[8] Reviewers have questioned the methodology of the trial.[9]
- ^ "Details for: Kengrexal". Health Canada. 30 November 2023. Retrieved 3 March 2024.
- ^ "Notice: Multiple Additions to the Prescription Drug List (PDL) [2023-03-08]". Health Canada. 8 March 2023. Retrieved 21 March 2023.
- ^ "Summary Basis of Decision for Kengrexal". Health Canada. 23 May 2023. Retrieved 5 June 2023.
- ^ "Kengreal- cangrelor injection, powder, lyophilized, for solution". DailyMed. 6 September 2022. Retrieved 3 March 2024.
- ^ a b Norgard NB, Hann CL, Dale GL (2009). "Cangrelor attenuates coated-platelet formation". Clinical and Applied Thrombosis/Hemostasis. 15 (2): 177–182. doi:10.1177/1076029608321437. PMID 18796456. S2CID 23639481.
- ^ CHAMPION Trials With Cangrelor Stopped for Lack of Efficacy
- ^ Napodano J (13 May 2009). "What Cangrelor Failure Means to Medicines". Seeking Alpha.
- ^ Bhatt DL, Stone GW, Mahaffey KW, Gibson CM, Steg PG, Hamm CW, et al. (April 2013). "Effect of platelet inhibition with cangrelor during PCI on ischemic events". The New England Journal of Medicine. 368 (14): 1303–1313. doi:10.1056/NEJMoa1300815. PMID 23473369.
- ^ Lange RA, Hillis LD (April 2013). "The duel between dual antiplatelet therapies". The New England Journal of Medicine. 368 (14): 1356–1357. doi:10.1056/NEJMe1302504. PMID 23473370.