This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these messages)
|
| Exocrine pancreatic insufficiency | |
|---|---|
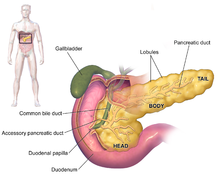 | |
| Anatomy of the pancreas | |
| Specialty | Endocrinology, gastroenterology |
| Causes | Diabetes (Type 2), Type 1 Diabetes, Pancreatitis, Celiac, Cystic Fibrosis, IBS-D, IBD, somatostatin analogues |
| Risk factors | older age, tobacco use, alcohol use |
| Diagnostic method | Fecal elastase test |
| Treatment | pancreatic enzyme replacement therapy (PERT) |
| Medication | pancrelipase |
Exocrine pancreatic insufficiency (EPI) is the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas. EPI can occur in humans and is prevalent in many conditions[1] such as cystic fibrosis,[2] Shwachman–Diamond syndrome,[3] different types of pancreatitis,[4] multiple types of diabetes mellitus (Type 1 and Type 2 diabetes),[5] advanced renal disease,[6] older adults,[7] celiac disease,[8] IBS-D,[9] IBD,[10] HIV,[11] alcohol-related liver disease,[12] Sjogren syndrome,[13] tobacco use,[14] and use of somatostatin analogues.[15]
EPI is caused by a progressive loss of the pancreatic cells that make digestive enzymes. Loss of digestive enzymes leads to maldigestion and malabsorption of nutrients from normal digestive processes. EPI can cause symptoms even before reaching the stages of malnutrition: 'mild' or 'moderate' EPI is when fecal elastase levels are <200 ug/g, whereas 'severe' EPI is considered to be when fecal elastase levels is <100 ug/g.[16]
The exocrine pancreas is a portion of this organ that contains clusters of ducts (acini) producing bicarbonate anion, a mild alkali, as well as an array of digestive enzymes that together empty by way of the interlobular and main pancreatic ducts into the duodenum (upper small intestine).[17] The hormones cholecystokinin and secretin secreted by the stomach and duodenum in response to distension and the presence of food in turn stimulate the production of digestive enzymes by the exocrine pancreas.[18] The alkalization of the duodenum neutralizes the acidic chyme produced by the stomach that is passing into it; the digestive enzymes serve to catalyze the breakdown of complex foodstuffs into smaller molecules for absorption and integration into metabolic pathways.[18] The enzymes include proteases (trypsinogen and chymotrypsinogen), hydrolytic enzymes that cleave lipids (the lipases phospholipase A2 and lysophospholipase, and cholesterol esterase), and amylase to digest starches. EPI results from progressive failure in the exocrine function of the pancreas to provide its digestive enzymes, often in response to a genetic condition or other disease state, resulting in the inability of the animal involved to properly digest food.[citation needed]
- ^ Capurso, Gabriele; Traini, Mariaemilia; Piciucchi, Matteo; Signoretti, Marianna; Arcidiacono, Paolo Giorgio (2019-12-31). "Exocrine pancreatic insufficiency: prevalence, diagnosis, and management". Clinical and Experimental Gastroenterology. 12: 129–139. doi:10.2147/CEG.S168266. PMC 6432881. PMID 30962702.
- ^ Ritivoiu, Mirela-Elena; Drăgoi, Cristina Manuela; Matei, Dumitru; Stan, Iustina Violeta; Nicolae, Alina Crenguţa; Craiu, Mihai; Dumitrescu, Ion-Bogdan; Ciolpan, Alina Angelica (3 January 2023). "Current and Future Therapeutic Approaches of Exocrine Pancreatic Insufficiency in Children with Cystic Fibrosis in the Era of Personalized Medicine". Pharmaceutics. 15 (1): 162. doi:10.3390/pharmaceutics15010162. PMC 9862205. PMID 36678791.
- ^ Nelson, Adam; Myers, Kasiani (1993), Adam, Margaret P.; Everman, David B.; Mirzaa, Ghayda M.; Pagon, Roberta A. (eds.), "Shwachman-Diamond Syndrome", GeneReviews®, Seattle (WA): University of Washington, Seattle, PMID 20301722, retrieved 2023-02-02
- ^ Ashraf, Hamza; Colombo, John Paul; Marcucci, Vincent; Rhoton, Jonathan; Olowoyo, Oluwatofunmi (2021-11-20). "A Clinical Overview of Acute and Chronic Pancreatitis: The Medical and Surgical Management". Cureus. 13 (11): e19764. doi:10.7759/cureus.19764. PMC 8684888. PMID 34938639.
- ^ Piciucchi, Matteo; Capurso, Gabriele; Archibugi, Livia; Delle Fave, Martina Maria; Capasso, Marina; Delle Fave, Gianfranco (2015). "Exocrine Pancreatic Insufficiency in Diabetic Patients: Prevalence, Mechanisms, and Treatment". International Journal of Endocrinology. 2015: 595649. doi:10.1155/2015/595649. PMC 4393909. PMID 25892991.
- ^ Griesche-Philippi, J.; Otto, J.; Schwörer, H.; Maisonneuve, P.; Lankisch, P.G. (December 2010). "Exocrine pancreatic function in patients with end-stage renal disease". Clinical Nephrology. 74 (12): 457–464. doi:10.5414/CNP74457. PMID 21084049.
- ^ Rothenbacher, Dietrich; Löw, Michael; Hardt, Philip D.; Klör, Hans-Ulrich; Ziegler, Hartwig; Brenner, Hermann (June 2005). "Prevalence and determinants of exocrine pancreatic insufficiency among older adults: Results of a population-based study". Scandinavian Journal of Gastroenterology. 40 (6): 697–704. doi:10.1080/00365520510023116. PMID 16036530.
- ^ Balaban, Daniel Vasile; Enache, Iulia; Ciochina, Marina; Popp, Alina; Jinga, Mariana (28 June 2022). "Pancreatic involvement in celiac disease". World Journal of Gastroenterology. 28 (24): 2680–2688. doi:10.3748/wjg.v28.i24.2680. PMC 9260863. PMID 35979168.
- ^ Olmos, Juan I.; Piskorz, María M.; Litwin, Nestor; Schaab, Sara; Tevez, Adriana; Bravo-Velez, Gladys; Uehara, Tatiana; Hashimoto, Harumi; Rey, Enzo; Sorda, Juan A.; Olmos, Jorge A. (December 2022). "Exocrine Pancreatic Insufficiency is Undiagnosed in Some Patients with Diarrhea-Predominant Irritable Bowel Syndrome Using the Rome IV Criteria". Digestive Diseases and Sciences. 67 (12): 5666–5675. doi:10.1007/s10620-022-07568-8. PMID 35704255.
- ^ Singh, Vikesh K.; Haupt, Mark E.; Geller, David E.; Hall, Jerry A.; Diez, Pedro M. Quintana (2017-10-21). "Less common etiologies of exocrine pancreatic insufficiency". World Journal of Gastroenterology. 23 (39): 7059–7076. doi:10.3748/wjg.v23.i39.7059. PMC 5656454. PMID 29093615.
- ^ Yilmaz, Aylin; Hagberg, Lars (4 March 2018). "Exocrine pancreatic insufficiency is common in people living with HIV on effective antiretroviral therapy". Infectious Diseases. 50 (3): 193–199. doi:10.1080/23744235.2017.1370126. PMID 28838283.
- ^ Leeds, John S.; Oppong, Kofi; Sanders, David S. (July 2011). "The role of fecal elastase-1 in detecting exocrine pancreatic disease". Nature Reviews Gastroenterology & Hepatology. 8 (7): 405–415. doi:10.1038/nrgastro.2011.91. PMID 21629239.
- ^ Ebert, Ellen Catherine (January 2012). "Gastrointestinal and Hepatic Manifestations of Sjogren Syndrome". Journal of Clinical Gastroenterology. 46 (1): 25–30. doi:10.1097/MCG.0b013e3182329d9c. PMID 22157220.
- ^ Raphael, Kara L.; Chawla, Saurabh; Kim, Sungjin; Keith, Christopher G.; Propp, David R.; Chen, Zhengjia N.; Woods, Kevin E.; Keilin, Steven A.; Cai, Qiang; Willingham, Field F. (February 2017). "Pancreatic Insufficiency Secondary to Tobacco Exposure: A Controlled Cross-Sectional Evaluation". Pancreas. 46 (2): 237–243. doi:10.1097/MPA.0000000000000721. PMC 6355146. PMID 27846134.
- ^ Lamarca, Angela; McCallum, Lynne; Nuttall, Christina; Barriuso, Jorge; Backen, Alison; Frizziero, Melissa; Leon, Rebecca; Mansoor, Was; McNamara, Mairéad G; Hubner, Richard A.; Valle, Juan W (2018-07-03). "Somatostatin analogue-induced pancreatic exocrine insufficiency in patients with neuroendocrine tumors: results of a prospective observational study". Expert Review of Gastroenterology & Hepatology. 12 (7): 723–731. doi:10.1080/17474124.2018.1489232. PMID 29923433.
- ^ Shandro, Benjamin M; Ritehnia, Jennifer; Chen, Joshua; Nagarajah, Rani; Poullis, Andrew (November 2020). "The investigation and management of pancreatic exocrine insufficiency: A retrospective cohort study". Clinical Medicine. 20 (6): 535–540. doi:10.7861/clinmed.2020-0506. PMC 7687321. PMID 33199316.
- ^ Pandol, Stephen J. (2010-01-01). Anatomy. Morgan & Claypool Life Sciences.
- ^ a b Pandol, Stephen J. (2010-01-01). Regulation of Whole-Organ Pancreatic Secretion. Morgan & Claypool Life Sciences.
