| Fertility awareness | |
|---|---|
 | |
| Background | |
| Type | Behavioral |
| First use | 1950s (mucus) mid-1930s (BBT) 1930 (Knaus-Ogino) Ancient (ad hoc) |
| Failure rates (first year) | |
| Perfect use | Symptothermal method: 0.4%[2] Ovulation method: 3%[2] TwoDay method: 4%[2] Standard Days method: 5%[2] |
| Typical use | Symptothermal method: 2% Ovulation Method: 11–34% TwoDay Method: 14% Standard Days Method: 11–14% Calendar Rhythm Method: 24%[3] |
| Usage | |
| Reversibility | Yes |
| User reminders | Dependent upon strict user adherence to methodology |
| Clinic review | None |
| Advantages and disadvantages | |
| STI protection | No |
| Periods | Increased prediction |
| Benefits | No side effects, can aid pregnancy achievement, personal self-awareness, greater marital intimacy |
Fertility awareness (FA) refers to a set of practices used to determine the fertile and infertile phases of a woman's menstrual cycle. Fertility awareness methods may be used to avoid pregnancy, to achieve pregnancy, or as a way to monitor gynecological health.
Methods of identifying infertile days have been known since antiquity, but scientific knowledge gained during the past century has increased the number, variety, and especially accuracy of methods.
Systems of fertility awareness rely on observation of changes in one or more of the primary fertility signs (basal body temperature, cervical mucus, and cervical position), tracking menstrual cycle length and identifying the fertile window based on this information, or both. Other signs may also be observed: these include breast tenderness and mittelschmerz (ovulation pains), urine analysis strips known as ovulation predictor kits (OPKs), and microscopic examination of saliva or cervical fluid. Also available are computerized fertility monitors.
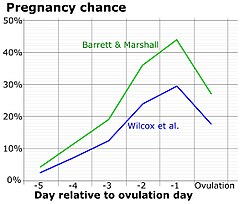
- ^ Dunson, D.B.; Baird, D.D.; Wilcox, A.J.; Weinberg, C.R. (1999). "Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation". Human Reproduction. 14 (7): 1835–1839. doi:10.1093/humrep/14.7.1835. ISSN 1460-2350. PMID 10402400.
- ^ a b c d Trussell, James (2011). "Contraceptive efficacy". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States. Archived 2017-02-15 at the Wayback Machine
- ^ Cite error: The named reference
Urrutia, Rachel Peragallo; Polis, Chelsea B. (2019-07-11)was invoked but never defined (see the help page).