| Fever | |
|---|---|
| Other names | Pyrexia, febrile response, febrile[1] |
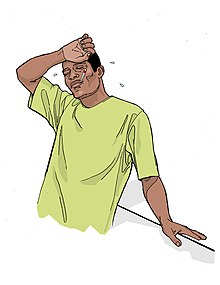 | |
| Person with fever | |
| Specialty | Infectious disease, pediatrics |
| Symptoms | Initially: shivering, feeling cold, chills[2] Later: flushed, sweating[3] |
| Complications | Febrile seizure[4] |
| Causes | Virus, bacteria, increase in the body's temperature set point[5][6] |
| Diagnostic method | Temperature higher than the normal range of 37.2 and 38.3 °C (99.0 and 100.9 °F)[1][7][8] |
| Differential diagnosis | Hyperthermia[1] |
| Treatment | Based on underlying cause, not required for fever itself[2][9] |
| Medication | Ibuprofen, paracetamol (acetaminophen)[9][10] |
| Frequency | Common[2][11] |
Fever or pyrexia in humans is a symptom of organism's anti-infection defense mechanism that appears with body temperature exceeding the normal range due to an increase in the body's temperature set point in the hypothalamus.[5][6][12][7] There is no single agreed-upon upper limit for normal temperature: sources use values ranging between 37.2 and 38.3 °C (99.0 and 100.9 °F) in humans.[1][7][8]
The increase in set point triggers increased muscle contractions and causes a feeling of cold or chills.[2] This results in greater heat production and efforts to conserve heat.[3] When the set point temperature returns to normal, a person feels hot, becomes flushed, and may begin to sweat.[3] Rarely a fever may trigger a febrile seizure, with this being more common in young children.[4] Fevers do not typically go higher than 41 to 42 °C (106 to 108 °F).[6]
A fever can be caused by many medical conditions ranging from non-serious to life-threatening.[13] This includes viral, bacterial, and parasitic infections—such as influenza, the common cold, meningitis, urinary tract infections, appendicitis, Lassa fever, COVID-19, and malaria.[13][14] Non-infectious causes include vasculitis, deep vein thrombosis, connective tissue disease, side effects of medication or vaccination, and cancer.[13][15] It differs from hyperthermia, in that hyperthermia is an increase in body temperature over the temperature set point, due to either too much heat production or not enough heat loss.[1]
Treatment to reduce fever is generally not required.[2][9] Treatment of associated pain and inflammation, however, may be useful and help a person rest.[9] Medications such as ibuprofen or paracetamol (acetaminophen) may help with this as well as lower temperature.[9][10] Children younger than three months require medical attention, as might people with serious medical problems such as a compromised immune system or people with other symptoms.[16] Hyperthermia requires treatment.[2]
Fever is one of the most common medical signs.[2] It is part of about 30% of healthcare visits by children[2] and occurs in up to 75% of adults who are seriously sick.[11] While fever evolved as a defense mechanism, treating a fever does not appear to improve or worsen outcomes.[17][18][19] Fever is often viewed with greater concern by parents and healthcare professionals than is usually deserved, a phenomenon known as "fever phobia."[2][20]
- ^ a b c d e Cite error: The named reference
NC08was invoked but never defined (see the help page). - ^ a b c d e f g h i Sullivan JE, Farrar HC (March 2011). "Fever and antipyretic use in children". Pediatrics. 127 (3): 580–587. doi:10.1542/peds.2010-3852. PMID 21357332.
- ^ a b c Huether, Sue E. (2014). Pathophysiology: The Biologic Basis for Disease in Adults and Children (7th ed.). Elsevier Health Sciences. p. 498. ISBN 978-0323293754.
- ^ a b CDC Staff (31 March 2020). "Taking Care of Someone Who is Sick: Caring for Someone Sick at Home". Archived from the original on 24 March 2015. Retrieved 8 May 2015.
- ^ a b Kluger MJ (2015). Fever: Its Biology, Evolution, and Function. Princeton University Press. p. 57. ISBN 978-1400869831.
- ^ a b c Garmel GM, Mahadevan SV, eds. (2012). "Fever in adults". An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 375. ISBN 978-0521747769.
- ^ a b c Dinarello CA, Porat R (2018). "Chapter 15: Fever". In Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo, J (eds.). Harrison's Principles of Internal Medicine. Vol. 1–2 (20th ed.). New York: McGraw-Hill. ISBN 9781259644030. Retrieved 31 March 2020.
- ^ a b Cite error: The named reference
CC09was invoked but never defined (see the help page). - ^ a b c d e Richardson M, Purssell E (September 2015). "Who's afraid of fever?". Archives of Disease in Childhood. 100 (9): 818–820. doi:10.1136/archdischild-2014-307483. PMID 25977564. S2CID 206857750.
- ^ a b Garmel GM, Mahadevan SV, eds. (2012). An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 401. ISBN 978-0521747769.
- ^ a b Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI (August 2013). "Fever effects and treatment in critical care: literature review". Australian Critical Care. 26 (3): 130–135. doi:10.1016/j.aucc.2012.10.004. PMID 23199670.
- ^ Franjić, Siniša (31 March 2019). "Fever Can Be A Symptom of Many Diseases". Journal of Medicine and HealthCare: 1–3. doi:10.47363/jmhc/2021(3)146. S2CID 243837498.
- ^ a b c Garmel GM, Mahadevan SV, eds. (2012). An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 5. ISBN 978-0521747769.
- ^ Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK, Franco-Paredes C (13 March 2020). "Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis". Travel Medicine and Infectious Disease. 34: 101623. doi:10.1016/j.tmaid.2020.101623. PMC 7102608. PMID 32179124.
- ^ Dayal R, Agarwal D (January 2016). "Fever in Children and Fever of Unknown Origin". Indian Journal of Pediatrics. 83 (1): 38–43. doi:10.1007/s12098-015-1724-4. PMID 25724501. S2CID 34481402.
- ^ "Fever". MedlinePlus. 30 August 2014. Archived from the original on 11 May 2009.
- ^ Schaffner A (March 2006). "Fieber – nützliches oder schädliches, zu behandelndes Symptom?" [Fever–useful or noxious symptom that should be treated?]. Therapeutische Umschau (in German). 63 (3): 185–188. doi:10.1024/0040-5930.63.3.185. PMID 16613288. Abstract alone is in German and in English.
- ^ Niven DJ, Stelfox HT, Laupland KB (June 2013). "Antipyretic therapy in febrile critically ill adults: A systematic review and meta-analysis". Journal of Critical Care. 28 (3): 303–310. doi:10.1016/j.jcrc.2012.09.009. PMID 23159136.
- ^ Ray, Juliet J. (December 2015). "Fever: suppress or let it ride?". Journal of Thoracic Disease. 7 (12): E633–E636. doi:10.3978/j.issn.2072-1439.2015.12.28. PMC 4703655. PMID 26793378.
- ^ Crocetti M, Moghbeli N, Serwint J (June 2001). "Fever Phobia Revisited: Have Parental Misconceptions About Fever Changed in 20 Years?". Pediatrics. 107 (6): 1241–1246. doi:10.1542/peds.107.6.1241. PMID 11389237.