| Naegleriasis | |
|---|---|
| Other names | Primary amoebic meningoencephalitis (PAM), amoebic encephalitis, naegleria infection, amoebic meningitis |
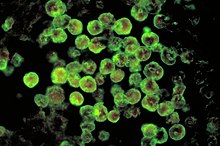 | |
| Histopathology, Direct fluorescent antibody stain. | |
| Pronunciation | |
| Specialty | Infectious disease |
| Symptoms | Fever, vomiting, stiff neck, seizures, poor coordination, confusion, death |
| Complications | Brain damage, death |
| Usual onset | 1 – 12 days after exposure[1] |
| Duration | 1 – 18 days[1] |
| Causes | Deep nasal inhalation of Naegleria fowleri organisms from contaminated freshwater. |
| Risk factors | Roughly 75% of cases infect males; most cases are children or adolescents[2] |
| Differential diagnosis | Bacterial or fungal meningitis[3] |
| Prevention | Noseclips when swimming in fresh water, or avoiding freshwater environments, and proper chlorination of swimming pools |
| Treatment | Miltefosine, fluconazole, amphotericin B, posaconazole, voriconazole, targeted temperature management[4][5] |
| Prognosis | 98.5% fatality rate; some, but not all, survivors have permanent neurological damage |
| Frequency | Extremely rare (6 in 1,000,000 human deaths, US) |
| Deaths | 381 globally from 1937–2018 |
Naegleriasis, also known as primary amoebic meningoencephalitis (PAM), is an almost invariably fatal infection of the brain by the free-living unicellular eukaryote Naegleria fowleri. Symptoms are meningitis-like and include headache, fever, nausea, vomiting, a stiff neck, confusion, hallucinations and seizures.[6] Symptoms progress rapidly over around five days, and death usually results within one to two weeks of symptoms.[6][1]
N. fowleri is typically found in warm bodies of fresh water, such as ponds, lakes, rivers and hot springs. It is found in an amoeboid, temporary flagellate stage or microbial cyst in soil, poorly maintained municipal water supplies, water heaters, near warm-water discharges of industrial plants and in poorly chlorinated or unchlorinated swimming pools. There is no evidence of it living in salt water. As the disease is rare, it is often not considered during diagnosis.[citation needed]
Although infection occurs very rarely,[1] it almost inevitably results in death.[7][8] Of the 128 naegleriasis US cases in the half-century to 2016, only two survived.[9]
- ^ a b c d "The Centers for Disease Control and Prevention, Division of Parasitic Diseases – Naegleria fowleri—Primary Amoebic Meningoencephalitis (PAM)—General Information". Archived from the original on 28 July 2018. Retrieved 26 May 2014.
- ^ Fortin, Jacey (25 July 2019). "Man Dies of 'Brain-Eating' Amoeba After Swimming in Lake". The New York Times. Archived from the original on 21 April 2020. Retrieved 1 April 2020.
- ^ Cite error: The named reference
MMWR2008was invoked but never defined (see the help page). - ^ Cite error: The named reference
CDC2015Txwas invoked but never defined (see the help page). - ^ Cite error: The named reference
Grace2015revwas invoked but never defined (see the help page). - ^ a b Cite error: The named reference
cdc.gov-2019was invoked but never defined (see the help page). - ^ "6 die from brain-eating amoeba after swimming". NBC News. Associated Press. 28 September 2007. Archived from the original on 2 September 2018. Retrieved 17 November 2019.
- ^ one death in September 2018 was the first confirmed case of the infection in the United States since 2016 (nytimes.com: A Man Died After Being Infected With a Brain-Eating Amoeba. Here Are the Facts Archived 31 July 2019 at the Wayback Machine)
- ^ Cohen, Elizabeth (23 August 2016). "Kali Hardig, brain-eating amoeba survivor, to begin school next week". CNN. Archived from the original on 23 December 2019.