| Paracoccidioidomycosis | |
|---|---|
| Other names | South American blastomycosis,[1] Brazilian blastomycosis,[2] Lutz-Splendore-de Almeida disease,[3] |
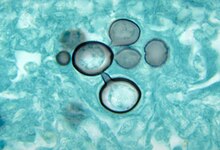 | |
| Paracoccidioides histopathology | |
| Specialty | Infectious disease |
| Symptoms | Fever, sepsis, weight loss, large glands, large liver and spleen,[4] mouth ulcers, skin lesions.[5] |
| Types | Mucocutaneous, lymphatic, multi-organ[1] |
| Causes | Paracoccidioides brasiliensis[4] |
| Diagnostic method | Sampling of blood, sputum, or skin[4] |
| Differential diagnosis | Tuberculosis, leukaemia, lymphoma[4] |
| Treatment | Antifungal medication[6] |
| Medication | Itraconazole, amphotericin B,[6] trimethoprim/sulfamethoxazole[7] |
| Deaths | 200 deaths per year in Brazil[1] |
Paracoccidioidomycosis (PCM), also known as South American blastomycosis, is a fungal infection that can occur as a mouth and skin type, lymphangitic type, multi-organ involvement type (particularly lungs), or mixed type.[1][6] If there are mouth ulcers or skin lesions, the disease is likely to be widespread.[1] There may be no symptoms, or it may present with fever, sepsis, weight loss, large glands, or a large liver and spleen.[4][7]
The cause is fungi in the genus Paracoccidioides, including Paracoccidioides brasiliensis and Paracoccidioides lutzii,[8] acquired by breathing in fungal spores.[6]
Diagnosis is by sampling of blood, sputum, or skin.[4] The disease can appear similar to tuberculosis, leukaemia, and lymphoma[4] Treatment is with antifungals; itraconazole.[1][7] For severe disease, treatment is with amphotericin B followed by itraconazole, or trimethoprim/sulfamethoxazole as an alternative.[1][7]
It is endemic to Central and South America,[9] and is considered a type of neglected tropical disease.[8] In Brazil, the disease causes around 200 deaths per year.[1]
- ^ a b c d e f g h James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2019). "13. Diseases resulting from fungi and yeasts". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier. pp. 313–314. ISBN 978-0-323-54753-6.
- ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007), Dermatology: 2-Volume Set, St. Louis: Mosby, ISBN 978-1-4160-2999-1
- ^ Cite error: The named reference
whowas invoked but never defined (see the help page). - ^ a b c d e f g "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 26 June 2021.
- ^ Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 451. ISBN 978-0-7020-6830-0.
- ^ a b c d Barlow, Gavin; Irving, Irving; moss, Peter J. (2020). "20. Infectious diseases". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 561. ISBN 978-0-7020-7870-5.
- ^ a b c d Proia, Laurie (2020). "28. The dimorphic mycoses". In Spec, Andrej; Escota, Gerome V.; Chrisler, Courtney; Davies, Bethany (eds.). Comprehensive Review of Infectious Diseases. Elsevier. pp. 419–420. ISBN 978-0-323-56866-1.
- ^ a b Queiroz-Telles, Flavio; Fahal, Ahmed Hassan; Falci, Diego R; Caceres, Diego H; Chiller, Tom; Pasqualotto, Alessandro C (November 2017). "Neglected endemic mycoses". The Lancet Infectious Diseases. 17 (11): e367–e377. doi:10.1016/S1473-3099(17)30306-7. PMID 28774696.(subscription required)
- ^ Marques, Silvio Alencar (October 2013). "Paracoccidioidomycosis: epidemiological, clinical, diagnostic and treatment up-dating". Anais Brasileiros de Dermatologia. 88 (5): 700–711. doi:10.1590/abd1806-4841.20132463. ISSN 0365-0596. PMC 3798345. PMID 24173174.