| Polycystic kidney disease | |
|---|---|
| Other names | Kidney - polycystic[1] |
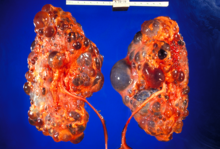 | |
| Severely affected polycystic kidneys removed at time of transplantation | |
| Specialty | Nephrology |
| Symptoms | Abdominal pain[1] |
| Types | ADPKD[2] and ARPKD[3] |
| Diagnostic method | MRI, CT scan, Ultrasound[1] |
| Treatment | Antihypertensives, Life style management[4] |
Polycystic kidney disease (PKD or PCKD, also known as polycystic kidney syndrome) is a genetic disorder[5][6] in which the renal tubules become structurally abnormal, resulting in the development and growth of multiple cysts within the kidney.[7] These cysts may begin to develop in utero, in infancy, in childhood, or in adulthood.[8] Cysts are non-functioning tubules filled with fluid pumped into them, which range in size from microscopic to enormous, crushing adjacent normal tubules and eventually rendering them non-functional as well.
PKD is caused by abnormal genes that produce a specific abnormal protein; this protein has an adverse effect on tubule development. PKD is a general term for two types, each having their own pathology and genetic cause: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD). The abnormal gene exists in all cells in the body; as a result, cysts may occur in the liver, seminal vesicles, and pancreas. This genetic defect can also cause aortic root aneurysms, and aneurysms in the circle of Willis cerebral arteries, which if they rupture, can cause a subarachnoid hemorrhage.
Diagnosis may be suspected from one, some, or all of the following: new onset flank pain or red urine; a positive family history; palpation of enlarged kidneys on physical exam; an incidental finding on abdominal sonogram; or an incidental finding of abnormal kidney function on routine lab work (BUN, serum creatinine, or eGFR). Definitive diagnosis is made by abdominal CT exam.
Complications include hypertension due to the activation of the renin–angiotensin–aldosterone system (RAAS), frequent cyst infections, urinary bleeding, and declining renal function. Hypertension is treated with angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). Infections are treated with antibiotics. Declining renal function is treated with renal replacement therapy (RRT): dialysis and/or transplantation. Management from the time of the suspected or definitive diagnosis is by an appropriately trained doctor.
- ^ a b c Cite error: The named reference
polywas invoked but never defined (see the help page). - ^ "Autosomal Dominant Polycystic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- ^ "Autosomal Recessive Polycystic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- ^ "What Is Polycystic Kidney Disease?". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- ^ Hildebrandt F (April 2010). "Genetic kidney diseases". Lancet. 375 (9722): 1287–1295. doi:10.1016/S0140-6736(10)60236-X. PMC 2898711. PMID 20382325.
- ^ Kimberling WJ, Pieke-Dahl SA, Kumar S (November 1991). "The genetics of cystic diseases of the kidney". Seminars in Nephrology. 11 (6): 596–606. PMID 1767134.
- ^ "polycystic kidney disease" at Dorland's Medical Dictionary
- ^ Cramer MT, Guay-Woodford LM (July 2015). "Cystic kidney disease: a primer". Advances in Chronic Kidney Disease. 22 (4): 297–305. doi:10.1053/j.ackd.2015.04.001. PMID 26088074.