| Typhoid fever | |
|---|---|
| Other names | Enteric fever, slow fever |
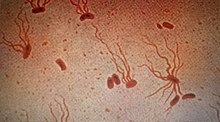 | |
| Causative agent: Salmonella enterica serological variant Typhi (shown under a microscope with flagellar stain) | |
| Specialty | Infectious diseases |
| Symptoms | Fever that starts low and increases daily, possibly reaching as high as 104.9 °F (40.5 °C) Headache, weakness and fatigue, muscle aches, sweating, dry cough, loss of appetite, weight loss, stomach pain, diarrhea or constipation, rash, swollen stomach (enlarged liver or spleen) |
| Usual onset | 1–2 weeks after ingestion |
| Duration | Usually 7–10 days after antibiotic treatment begins. Longer if there are complications or drug resistance. |
| Causes | Gastrointestinal infection of Salmonella enterica serotype Typhi |
| Risk factors | Living in or travel to areas where typhoid fever is established; work as a clinical microbiologist handling Salmonella Typhi bacteria; have close contact with someone who is infected or has recently been infected with typhoid fever; drink water polluted by sewage that contains Salmonella Typhi |
| Prevention | Preventable by vaccine. Travelers to regions with higher typhoid prevalence are usually encouraged to get a vaccination before travel. |
| Treatment | Antibiotics, hydration, surgery in extreme cases. Quarantine to avoid exposing others (not commonly done in modern times). |
| Prognosis | Likely to recover without complications if proper antibiotics administered and diagnosed early. If infecting strain is multi-drug resistant or extensively drug resistant then prognosis more difficult to determine.
Among untreated acute cases, 10% will shed bacteria for three months after initial onset of symptoms, and 2–5% will become chronic typhoid carriers.[1] Some carriers are diagnosed by positive tissue specimen. Chronic carriers are by definition asymptomatic.[1] |
Typhoid fever, also known simply as typhoid, is a disease caused by Salmonella enterica serotype Typhi bacteria, also called Salmonella typhi.[2][3] Symptoms vary from mild to severe, and usually begin six to 30 days after exposure.[4][5] Often there is a gradual onset of a high fever over several days.[4] This is commonly accompanied by weakness, abdominal pain, constipation, headaches, and mild vomiting.[6][5][7] Some people develop a skin rash with rose colored spots.[5] In severe cases, people may experience confusion.[7] Without treatment, symptoms may last weeks or months.[5] Diarrhea may be severe, but is uncommon.[7] Other people may carry it without being affected, but are still contagious.[8] Typhoid fever is a type of enteric fever, along with paratyphoid fever.[2] Salmonella enterica Typhi is believed to infect and replicate only within humans.[9]
Typhoid is caused by the bacterium Salmonella enterica subsp. enterica serovar Typhi growing in the intestines, Peyer's patches, mesenteric lymph nodes, spleen, liver, gallbladder, bone marrow and blood.[5][7] Typhoid is spread by eating or drinking food or water contaminated with the feces of an infected person.[8] Risk factors include limited access to clean drinking water and poor sanitation.[2] Those who have not yet been exposed to it and ingest contaminated drinking water or food are most at risk for developing symptoms.[7] Only humans can be infected; there are no known animal reservoirs.[8] Salmonella Typhi which causes typhoid fever is different than the other Salmonella bacteria that usually cause salmonellosis, a common type of food poisoning.[10]
Diagnosis is performed by culturing and identifying S. enterica typhi from patient samples or detecting an immune response to the pathogen from blood samples.[5][2][11] Recently, new advances in large-scale data collection and analysis have allowed researchers to develop better diagnostics, such as detecting changing abundances of small molecules in the blood that may specifically indicate typhoid fever.[12] Diagnostic tools in regions where typhoid is most prevalent are quite limited in their accuracy and specificity, and the time required for a proper diagnosis, the increasing spread of antibiotic resistance, and the cost of testing are also hardships for under-resourced healthcare systems.[9]
A typhoid vaccine can prevent about 40–90% of cases during the first two years.[13] The vaccine may have some effect for up to seven years.[2] For those at high risk or people traveling to areas where it is common, vaccination is recommended.[8] Other efforts to prevent it include providing clean drinking water, good sanitation, and handwashing.[5][8] Until an infection is confirmed as cleared, the infected person should not prepare food for others.[5] Typhoid is treated with antibiotics such as azithromycin, fluoroquinolones, or third-generation cephalosporins.[2] Resistance to these antibiotics has been developing, which has made treatment more difficult.[2][14][15]
In 2015, 12.5 million new typhoid cases were reported.[16] The disease is most common in India.[2] Children are most commonly affected.[2][8] Typhoid decreased in the developed world in the 1940s as a result of improved sanitation and the use of antibiotics.[8] Every year about 400 cases are reported in the U.S. and an estimated 6,000 people have typhoid.[7][17] In 2015, it resulted in about 149,000 deaths worldwide – down from 181,000 in 1990.[18][19] Without treatment, the risk of death may be as high as 20%.[8] With treatment, it is between 1% and 4%.[2][8]
Typhus is a different disease, caused by unrelated species of bacteria.[20] Owing to their similar symptoms, they were not recognized as distinct diseases until the 1800s. "Typhoid" means "resembling typhus".[21]
- ^ a b "TYPHOID FEVER, ACUTE AND CARRIER" (PDF). Acute Communicable Disease Control: 2016 Annual Morbidity Report. 2016. p. 133 – via Los Angeles County Department of Public Health.
- ^ a b c d e f g h i j Wain J, Hendriksen RS, Mikoleit ML, Keddy KH, Ochiai RL (March 2015). "Typhoid fever". Lancet. 385 (9973): 1136–45. doi:10.1016/s0140-6736(13)62708-7. PMID 25458731. S2CID 2409150.
- ^ Mathur R, Oh H, Zhang D, Park SG, Seo J, Koblansky A, et al. (October 2012). "A Mouse Model of Salmonella Typhi Infection". Cell. 151 (3): 590–602. doi:10.1016/j.cell.2012.08.042. ISSN 0092-8674. PMC 3500584. PMID 23101627.
- ^ a b Newton AE (2014). "3 Infectious Diseases Related To Travel". CDC health information for international travel 2014: the yellow book. Oup USA. ISBN 978-0-19-994849-9. Archived from the original on 2015-07-02.
- ^ a b c d e f g h "Typhoid Fever". cdc.gov. May 14, 2013. Archived from the original on 6 June 2016. Retrieved 28 March 2015.
- ^ "Typhoid". www.who.int. Retrieved 2024-05-18.
- ^ a b c d e f "Typhoid Fever". cdc.gov. May 14, 2013. Archived from the original on 2 April 2015. Retrieved 28 March 2015.
- ^ a b c d e f g h i "Typhoid vaccines: WHO position paper" (PDF). Relevé Épidémiologique Hebdomadaire. 83 (6): 49–59. February 2008. PMID 18260212. Archived from the original (PDF) on April 2, 2015.
- ^ a b Pitzer VE, Meiring J, Martineau FP, Watson CH, Kang G, Basnyat B, et al. (October 2019). "The Invisible Burden: Diagnosing and Combatting Typhoid Fever in Asia and Africa". Clinical Infectious Diseases. 69 (Suppl 5): S395–S401. doi:10.1093/cid/ciz611. PMC 6792124. PMID 31612938.
- ^ "Typhoid Fever: Causes, Symptoms & Treatment".
- ^ Crump JA, Mintz ED (January 2010). "Global trends in typhoid and paratyphoid Fever". Clinical Infectious Diseases. 50 (2): 241–6. doi:10.1086/649541. PMC 2798017. PMID 20014951.
- ^ Näsström E, Parry CM, Thieu NT, Maude RR, de Jong HK, Fukushima M, et al. (2017). Reproducible diagnostic metabolites in plasma from typhoid fever patients in Asia and Africa. Umeå universitet, Kemiska institutionen. OCLC 1234663430.
- ^ Milligan R, Paul M, Richardson M, Neuberger A (May 2018). "Vaccines for preventing typhoid fever". The Cochrane Database of Systematic Reviews. 2018 (5): CD001261. doi:10.1002/14651858.CD001261.pub4. PMC 6494485. PMID 29851031.
- ^ Chatham-Stephens K, Medalla F, Hughes M, Appiah GD, Aubert RD, Caidi H, et al. (January 2019). "Emergence of Extensively Drug-Resistant Salmonella Typhi Infections Among Travelers to or from Pakistan – United States, 2016–2018". MMWR. Morbidity and Mortality Weekly Report. 68 (1): 11–13. doi:10.15585/mmwr.mm6801a3. PMC 6342547. PMID 30629573.
- ^ Kuehn R, Stoesser N, Eyre D, Darton TC, Basnyat B, Parry CM (24 November 2022). "Treatment of enteric fever (typhoid and paratyphoid fever) with cephalosporins". Cochrane Database of Systematic Reviews. 2022 (11): CD010452. doi:10.1002/14651858.CD010452.pub2. PMC 9686137. PMID 36420914.
- ^ Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ Jackson BR, Iqbal S, Mahon B (March 2015). "Updated recommendations for the use of typhoid vaccine—Advisory Committee on Immunization Practices, United States, 2015". MMWR. Morbidity and Mortality Weekly Report. 64 (11): 305–8. PMC 4584884. PMID 25811680.
- ^ Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Abubakar II, Tillmann T, Banerjee A, et al. (GBD 2013 Mortality and Causes of Death Collaborators) (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ^ Cunha BA (March 2004). "Osler on typhoid fever: differentiating typhoid from typhus and malaria". Infectious Disease Clinics of North America. 18 (1): 111–25. doi:10.1016/S0891-5520(03)00094-1. PMID 15081508.
- ^ Evans AS, Brachman PS (2013). Bacterial Infections of Humans: Epidemiology and Control. Springer. p. 839. ISBN 978-1-4615-5327-4.