| Vaginal epithelium | |
|---|---|
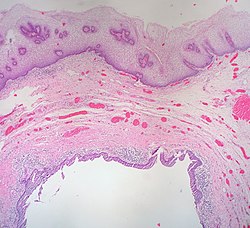 The epithelium of the vagina, visible at top, consists of multiple layers of flat cells. | |
| Details | |
| Part of | Vagina |
| Anatomical terminology | |
| This article is part of a series on |
| Epithelia |
|---|
| Squamous epithelial cell |
| Columnar epithelial cell |
| Cuboidal epithelial cell |
| Specialised epithelia |
|
| Other |
The vaginal epithelium is the inner lining of the vagina consisting of multiple layers of (squamous) cells.[1][2][3] The basal membrane provides the support for the first layer of the epithelium-the basal layer. The intermediate layers lie upon the basal layer, and the superficial layer is the outermost layer of the epithelium.[4][5] Anatomists have described the epithelium as consisting of as many as 40 distinct layers of cells.[6][7] The mucus found on the epithelium is secreted by the cervix and uterus.[8] The rugae of the epithelium create an involuted surface and result in a large surface area that covers 360 cm2.[9] This large surface area allows the trans-epithelial absorption of some medications via the vaginal route.
In the course of the reproductive cycle, the vaginal epithelium is subject to normal, cyclic changes, that are influenced by estrogen: with increasing circulating levels of the hormone, there is proliferation of epithelial cells along with an increase in the number of cell layers.[10][11] As cells proliferate and mature, they undergo partial cornification.[9][12] Although hormone induced changes occur in the other tissues and organs of the female reproductive system, the vaginal epithelium is more sensitive and its structure is an indicator of estrogen levels.[11][12][13] Some Langerhans cells and melanocytes are also present in the epithelium.[12] The epithelium of the ectocervix is contiguous with that of the vagina, possessing the same properties and function.[14] The vaginal epithelium is divided into layers of cells, including the basal cells, the parabasal cells, the superficial squamous flat cells, and the intermediate cells.[15][16][8] The superficial cells exfoliate continuously, and basal cells replace the superficial cells that die and slough off from the stratum corneum.[17][18][19] Under the stratus corneum is the stratum granulosum and stratum spinosum.[20] The cells of the vaginal epithelium retain a usually high level of glycogen compared to other epithelial tissue in the body.[21] The surface patterns on the cells themselves are circular and arranged in longitudinal rows.[7] The epithelial cells of the uterus possess some of the same characteristics of the vaginal epithelium.[22]
- ^ Up to 26 layers have been seen - see Pathology, American Society for Colposcopy and Cervical; Mayeaux, E. J.; Cox, J. Thomas (2011-12-28). Modern Colposcopy Textbook and Atlas. Lippincott Williams & Wilkins. ISBN 9781451153835.
- ^ E R, Weissenbacher (2015-06-02). Immunology of the female genital tract. Heidelberg. p. 16. ISBN 9783642149054. OCLC 868922790.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Hafez ES, Kenemans P (2012-12-06). Atlas of Human Reproduction: By Scanning Electron Microscopy. Springer Science & Business Media. ISBN 9789401181402.
- ^ Cite error: The named reference
Brownwas invoked but never defined (see the help page). - ^ Cite error: The named reference
Arulkumaranwas invoked but never defined (see the help page). - ^ Anderson, Deborah J.; Marathe, Jai; Pudney, Jeffrey (2014). "The Structure of the Human Vaginal Stratum Corneum and its Role in Immune Defense". American Journal of Reproductive Immunology. 71 (6): 618–623. doi:10.1111/aji.12230. ISSN 1046-7408. PMC 4024347. PMID 24661416.
- ^ a b Hafez ES, Kenemans P (2012-12-06). Atlas of Human Reproduction: By Scanning Electron Microscopy. Springer Science & Business Media. pp. 1–6. ISBN 9789401181402.
- ^ a b USMLE Step 1 Lecture Notes 2017: Anatomy. Simon and Schuster. 2017. p. 185. ISBN 9781506209463.
- ^ a b Anderson DJ, Marathe J, Pudney J (June 2014). "The structure of the human vaginal stratum corneum and its role in immune defense". American Journal of Reproductive Immunology. 71 (6): 618–23. doi:10.1111/aji.12230. PMC 4024347. PMID 24661416.
- ^ Nauth HF (2014). Gynäkologische Zytodiagnostik (in German) (2nd ed.). Stuttgart: Georg Thieme. p. 22. ISBN 978-3-13-131092-7.
- ^ a b Karl Knörr, Henriette Knörr-Gärtner, Fritz K. Beller, Christian Lauritzen (2013), Geburtshilfe und Gynäkologie: Physiologie und Pathologie der Reproduktion (in German) (3rd ed.), Berlin: Springer, pp. 24–25, ISBN 978-3-642-95584-6
{{citation}}: CS1 maint: multiple names: authors list (link) - ^ a b c Pathology AS, Mayeaux EJ, Cox JT (2011-12-28). Modern Colposcopy Textbook and Atlas. Lippincott Williams & Wilkins. ISBN 9781451153835.
- ^ "Vaginal Cytology: Introduction and Index". www.vivo.colostate.edu. Retrieved 2018-02-06.
- ^ Cite error: The named reference
:1was invoked but never defined (see the help page). - ^ Dutta DC, Konar H (2014-04-30). DC Dutta's Textbook of Gynecology. JP Medical Ltd. ISBN 9789351520689.
- ^ Mayeaux EJ, Cox TJ (2011). Modern Colposcopy Textbook and Atlas. Lippincott Williams & Wilkins. ISBN 978-1451153835. Retrieved December 11, 2017.
- ^ Beckmann CR (2010). Obstetrics and Gynecology. Lippincott Williams & Wilkins. pp. 241–245. ISBN 978-0781788076.
- ^ Kurman RJ, ed. (2002). Blaustein's Pathology of the Female Genital Tract (5th ed.). Springer. p. 154. ISBN 9780387952031.
- ^ Stanley J. Robboy (2009). Robboy's Pathology of the Female Reproductive Tract. Elsevier Health Sciences. p. 111. ISBN 978-0443074776. Retrieved November 5, 2014.
- ^ Haschek WM, Rousseaux CG, Wallig MA (2009-11-23). Fundamentals of Toxicologic Pathology. Academic Press. ISBN 9780080919324.
- ^ Kurman RJ, ed. (2002). Blaustein's Pathology of the Female Genital Tract (5th ed.). Springer. p. 154. ISBN 9780387952031.
- ^ Yarbrough, Victoria L.; Winkle, Sean; Herbst-Kralovetz, Melissa M. (2015-05-01). "Antimicrobial peptides in the female reproductive tract: a critical component of the mucosal immune barrier with physiological and clinical implications (review)". Human Reproduction Update. 21 (3): 353–377. doi:10.1093/humupd/dmu065. ISSN 1355-4786. PMID 25547201.