| Vaginal yeast infection | |
|---|---|
| Other names | Candidal vulvovaginitis, vaginal thrush |
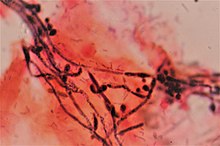 | |
| Gram stain showing the spores and pseudohyphae of Candida albicans surrounded by round vaginal skin cells, in a case of candidal vulvovaginitis. | |
| Specialty | Gynaecology |
| Symptoms | Vaginal itching, burning with urination, white and thick vaginal discharge, pain with sex, redness around the vagina[1] |
| Causes | Excessive growth of Candida[1] |
| Risk factors | Antibiotics, pregnancy, diabetes, HIV/AIDS[2] |
| Diagnostic method | Testing the vaginal discharge[1] |
| Differential diagnosis | Chlamydia, gonorrhea, bacterial vaginosis[3][1] |
| Treatment | Antifungal medication[4] |
| Frequency | 75% of women at some point[1] |
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation.[5][1] The most common symptom is vaginal itching, which may be severe.[1] Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina.[1] Symptoms often worsen just before a woman's period.[2]
Vaginal yeast infections are due to excessive growth of Candida.[1] These yeast are normally present in the vagina in small numbers.[1] Vaginal yeast infections are typically caused by the yeast species Candida albicans. Candida albicans is a common fungus often harbored in the mouth, digestive tract, or vagina without causing adverse symptoms.[6] The causes of excessive Candida growth are not well understood,[7] but some predisposing factors have been identified.
It is not classified as a sexually transmitted infection; however, it may occur more often in those who are frequently sexually active.[1][2] Risk factors include taking antibiotics, pregnancy, diabetes, and HIV/AIDS.[2] Tight clothing, type of underwear, and personal hygiene do not appear to be factors.[2] Diagnosis is by testing a sample of vaginal discharge.[1] As symptoms are similar to that of the sexually transmitted infections, chlamydia and gonorrhea, testing may be recommended.[1]
Treatment is with an antifungal medication.[4] This may be either as a cream such as clotrimazole or with oral medications such as fluconazole.[4] Despite the lack of evidence, wearing cotton underwear and loose fitting clothing is often recommended as a preventive measure.[1][2] Avoiding douching and scented hygiene products is also recommended.[1] Probiotics have not been found to be useful for active infections.[8]
Around 75% of women have at least one vaginal yeast infection at some point in their lives, while nearly half have at least two.[1][9] Around 5% have more than three infections in a single year.[9] It is the second most common cause of vaginal inflammation after bacterial vaginosis.[3]
- ^ a b c d e f g h i j k l m n o p "Vaginal yeast infections fact sheet". womenshealth.gov. December 23, 2014. Archived from the original on 4 March 2015. Retrieved 5 March 2015.
- ^ a b c d e f Sobel JD (June 2007). "Vulvovaginal candidosis". Lancet. 369 (9577): 1961–1971. doi:10.1016/S0140-6736(07)60917-9. PMID 17560449. S2CID 33894309.
- ^ a b Ilkit M, Guzel AB (August 2011). "The epidemiology, pathogenesis, and diagnosis of vulvovaginal candidosis: a mycological perspective". Critical Reviews in Microbiology. 37 (3): 250–261. doi:10.3109/1040841X.2011.576332. PMID 21599498. S2CID 19328371.
- ^ a b c Workowski KA, Berman SM (August 2006). "Sexually transmitted diseases treatment guidelines, 2006". MMWR. Recommendations and Reports. 55 (RR-11): 1–94. PMID 16888612. Archived from the original on 2014-10-20.
- ^ James WD, Berger TG, Elston DM (2006). Andrews' Diseases of the Skin: clinical Dermatology (10th ed.). Saunders Elsevier. p. 309. ISBN 978-0-7216-2921-6.
- ^ "Vaginal yeast infection". MedlinePlus. National Institutes of Health. Archived from the original on 4 April 2015. Retrieved 14 May 2015.
- ^ Watson CJ, Grando D, Garland SM, Myers S, Fairley CK, Pirotta M (November 2012). "Premenstrual vaginal colonization of Candida and symptoms of vaginitis". Journal of Medical Microbiology. 61 (Pt 11): 1580–1583. doi:10.1099/jmm.0.044578-0. PMID 22837219.
- ^ Abad CL, Safdar N (June 2009). "The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review". Journal of Chemotherapy. 21 (3): 243–252. doi:10.1179/joc.2009.21.3.243. PMID 19567343. S2CID 32398416.
- ^ a b Egan ME, Lipsky MS (September 2000). "Diagnosis of vaginitis". American Family Physician. 62 (5): 1095–1104. PMID 10997533. Archived from the original on 2011-06-06.