| Achalasia microcephaly | |
|---|---|
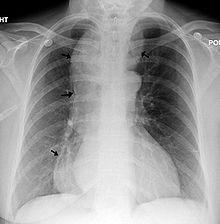 | |
| Chest x-ray of an individual with achalasia. The arrows point to the areas of extreme esophageal dilation. | |
| Symptoms | Manifestation of achalasia: regurgitation, vomiting and dysphagia, alongside diagnosis of microcephaly: abnormally small head size below the third percentile as well as mild to moderate mental retardation. |
| Frequency | 9 children between 1980-2017 |
Achalasia microcephaly syndrome is a rare condition whereby achalasia in the oesophagus manifests alongside microcephaly and intellectual disability. This is a rare constellation of symptoms with a predicted familial trend.[1]
The main signs of achalasia microcephaly syndrome involve the manifestation of each individual disease associated with the condition. Microcephaly can be primary, where the brain fails to develop properly during pregnancy, or secondary, where the brain is normal sized at birth but fails to grow as the child ages.[2] Abnormalities will be observed progressively after birth whereby the child will display stunted growth and physical and cognitive development. The occipital-frontal circumference will be at or near the extreme lower end, the third percentile, indicating microcephaly.[3] There are both genetic and behavioural causes of microcephaly.[2]
Achalasia, or oesophageal achalasia, is a disorder occurring in the lower oesophageal sphincter (LES). The LES fails to relax completely, resulting in frequent vomiting and regurgitation, usually one to two hours after meals.[4][3] If untreated, the long-term health of the individual will be compromised, leading to the development of dysphagia, weight loss and chronic aspiration.[4] It is very rare in children, especially siblings.[3] Mortality, specifically in young children, can occur.[3]
Due to the nature of the individual diseases, there is no cure for achalasia microcephaly. Treatment for achalasia involves drugs and surgical intervention, such as heller myotomy, with the goal of relieving LES pressure and its symptoms. Management of these symptoms are important for the maintenance of the quality of life of the child and the prevention of the progression to more serious complications. These include organ perforation, aspiration pneumonia and death.[4][5][6] Similarly, there is no cure for microcephaly and instead, early intervention, such as speech and physical therapy is recommended[7] Families who have a genetic predisposition to microcephaly can involve genetic counselling in their planning for pregnancy[8]
As of 2017[update], there are 5 reported cases of achalasia microcephaly syndrome, all of which involve children.[6]
- ^ Gockel HR, Schumacher J, Gockel I, Lang H, Haaf T, Nöthen MM (October 2010). "Achalasia: will genetic studies provide insights?". Human Genetics. 128 (4): 353–64. doi:10.1007/s00439-010-0874-8. PMID 20700745. S2CID 583462.
- ^ a b Woods CG (February 2004). "Human microcephaly". Current Opinion in Neurobiology. 14 (1): 112–7. doi:10.1016/j.conb.2004.01.003. PMID 15018946. S2CID 30096852.
- ^ a b c d Khalifa MM (October 1988). "Familial achalasia, microcephaly, and mental retardation. Case report and review of literature". Clinical Pediatrics. 27 (10): 509–12. doi:10.1177/000992288802701009. PMID 3048841. S2CID 40020496.
- ^ a b c Spiess, A.E; Kahrilas, P.J (1998). "Treating achalasia: from whalebone to laparoscope". Journal of the American Medical Association. 280 (7): 638–642. doi:10.1001/jama.280.7.638. PMID 9718057.
- ^ Pohl, D; Tutuian, R (2007). "Achalasia: an Overview of Diagnosis and Treatment". Journal of Gastrointestinal and Liver Diseases. 16 (3): 297–303. PMID 17925926. Archived from the original on 2019-05-11. Retrieved 2019-05-27.
- ^ a b Wafik M, Kini U (July 2017). "Achalasia-microcephaly syndrome: a further case report". Clinical Dysmorphology. 26 (3): 190–192. doi:10.1097/MCD.0000000000000181. PMID 28471776. S2CID 3694526.
- ^ "Microcephaly Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". 2016-03-11. Archived from the original on 2016-03-11. Retrieved 2019-05-27.
- ^ Hollander, N.S.D.; Wessels, M.W.; Los, F.J.; Ursem, N.T.C.; Niermeijer, M.F.; Wladimiroff, J.W. (2000). "Congenital microcephaly detected by prenatal ultrasound: genetic aspects and clinical significance" (PDF). Ultrasound in Obstetrics and Gynecology. 15 (4): 282–287. doi:10.1046/j.1469-0705.2000.00092.x. ISSN 0960-7692. PMID 10895445.