| Acute limb ischaemia | |
|---|---|
| Other names | Acute limb ischemia |
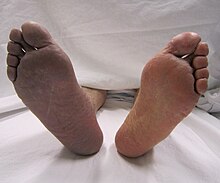 | |
| Acute embolism to the right femoral artery resulting in ischemia | |
| Symptoms | Cold, painful, pulseless limb that cannot move |
| Causes | Embolism, thrombosis |
| Treatment | Thrombectomy, embolectomy, thrombolysis |
| Medication | Thrombolytic drugs |
Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb[1] within 14 days of symptoms onset.[2] On the other hand, when the symptoms exceed 14 days,[3] it is called critical limb ischemia (CLI). CLI is the end stage of peripheral vascular disease where there is still some collateral circulation (alternate circulation pathways) that bring some blood flow (although inadequate) to the distal parts of the limbs.[2] While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss, whereas ALI is a vascular emergency.[4]
Acute limb ischaemia is usually caused by embolism or thrombosis, or rarely by dissection or trauma.[5] Thrombosis is usually caused by peripheral vascular disease (atherosclerotic disease that leads to blood vessel blockage), while an embolism is usually of cardiac origin.[6] In the United States, ALI is estimated to occur in 14 out of every 100,000 people per year.[7] With proper surgical care, acute limb ischaemia is a highly treatable condition; however, delayed treatment (beyond 6 to 12 hours) can result in permanent disability, amputation, and/or death. Early detection and steps towards fixing the problem with limb-sparing techniques can salvage the limb. Compartment syndrome is an occasional complication that may also occur in acute limb ischaemia because of the biotoxins that accumulate distal to the occlusion resulting in edema.[1]
- ^ a b Walker T. Gregory (2009). "Acute Limb Ischemia". Techniques in Vascular and Interventional Radiology. 12 (2): 117–129. doi:10.1053/j.tvir.2009.08.005. PMID 19853229.
- ^ a b Olinic DM, Stanek A, Tătaru DA, Homorodean C, Olinic M (August 2019). "Acute Limb Ischemia: An Update on Diagnosis and Management". Journal of Clinical Medicine. 8 (8): 1215. doi:10.3390/jcm8081215. PMC 6723825. PMID 31416204.
- ^ Fabiani I, Calogero E, Pugliese NR, Di Stefano R, Nicastro I, Buttitta F, Nuti M, Violo C, Giannini D, Morgantini A, Conte L, Barletta V, Berchiolli R, Adami D, Ferrari M, Di Bello V (July 2018). "Critical Limb Ischemia: A Practical Up-To-Date Review". Angiology. 69 (6): 465–474. doi:10.1177/0003319717739387. PMID 29161885. S2CID 22281024.
- ^ Farber, A (12 July 2018). "Chronic Limb-Threatening Ischemia". The New England Journal of Medicine. 379 (2): 171–180. doi:10.1056/NEJMcp1709326. PMID 29996085. S2CID 51623293.
- ^ Creager, Mark A.; Kaufman, John A.; Conte, Michael S. (2012). "Acute Limb Ischemia". New England Journal of Medicine. 366 (23): 2198–2206. doi:10.1056/NEJMcp1006054. PMID 22670905.
- ^ Klonaris, C; Georgopoulos, S; Katsargyris, A; Tsekouras, N; Bakoyiannis, C; Giannopoulos, A; Bastounis, E (March 2007). "Changing patterns in the etiology of acute lower limb ischemia". International Angiology. 26 (1): 49–52. PMID 17353888.
- ^ Dormandy J, Heeck L, Vig S (June 1999). "Acute limb ischemia". Semin Vasc Surg. 12 (2): 148–53. PMID 10777242.