| Central pontine myelinolysis | |
|---|---|
| Other names | Osmotic demyelination syndrome, central pontine demyelination |
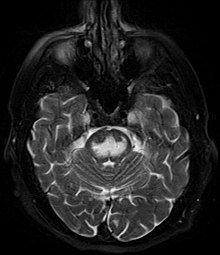 | |
| Axial fat-saturated T2-weighted image showing hyperintensity in the pons with sparing of the peripheral fibers, the patient was an alcoholic admitted with a serum Na of 101 treated with hypertonic saline, he was left with quadriparesis, dysarthria, and altered mental status | |
| Specialty | Neurology |
| Causes | Alcoholism, malnutrition |
Central pontine myelinolysis is a neurological condition involving severe damage to the myelin sheath of nerve cells in the pons (an area of the brainstem). It is predominately iatrogenic (treatment-induced), and is characterized by acute paralysis, dysphagia (difficulty swallowing), dysarthria (difficulty speaking), and other neurological symptoms.
Central pontine myelinolysis was first described as a disorder in 1959. The original paper[1] described four cases with fatal outcomes, and the findings on autopsy. The disease was described as a disease of alcoholics and malnutrition.[2] 'Central pontine' indicated the site of the lesion and 'myelinolysis' was used to emphasise that myelin was affected. The authors intentionally avoided the term 'demyelination' to describe the condition, in order to differentiate this condition from multiple sclerosis and other neuroinflammatory disorders.[3]
Since this original description, demyelination in other areas of the central nervous system associated with osmotic stress has been described outside the pons (extrapontine).[4] Osmotic demyelination syndrome is the term used for both central pontine myelinolysis and extrapontine myelinolysis.[5]
Central pontine myelinolysis, and osmotic demyelination syndrome, present most commonly as a complication of treatment of patients with profound hyponatremia (low sodium), which can result from a varied spectrum of conditions, based on different mechanisms. It occurs as a consequence of a rapid rise in serum tonicity following treatment in individuals with chronic, severe hyponatremia who have made intracellular adaptations to the prevailing hypotonicity.[6][7]
- ^ Adams RD, Victor M, Mancall EL (1959). "Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients". AMA Arch Neurol Psychiatry. 81 (2): 154–72. doi:10.1001/archneurpsyc.1959.02340140020004. PMID 13616772.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cite error: The named reference
Yoonwas invoked but never defined (see the help page). - ^ Bose P, Kunnacherry A, Maliakal P (September 2011). "Central pontine myelinolysis without hyponatraemia". The Journal of the Royal College of Physicians of Edinburgh. 41 (3): 211–214. doi:10.4997/JRCPE.2011.305. PMID 21949915.
- ^ Gocht A, Colmant HJ (1987). "Central pontine and extrapontine myelinolysis: a report of 58 cases". Clinical Neuropathology. 6 (6): 262–270. PMID 3322623.
- ^ Lampl C, Yazdi K (2002). "Central pontine myelinolysis". European Neurology. 47 (1): 3–10. doi:10.1159/000047939. PMID 11803185. S2CID 46885398. Archived from the original on 2012-03-06.
- ^ Babar SM (October 2013). "SIADH associated with ciprofloxacin". The Annals of Pharmacotherapy. 47 (10): 1359–1363. doi:10.1177/1060028013502457. PMID 24259701. S2CID 36759747.
- ^ Yoon B, Shim YS, Chung SW (2008). "Central pontine and extrapontine myelinolysis after alcohol withdrawal". Alcohol and Alcoholism. 43 (6): 647–649. doi:10.1093/alcalc/agn050. PMID 18678596.