| Contracture | |
|---|---|
 | |
| Specialty | Orthopedics |

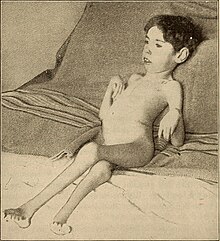
In pathology, a contracture is a shortening of muscles, tendons, skin, and nearby soft tissues that causes the joints to shorten and become very stiff, preventing normal movement.[1][2] A contracture is usually permanent, but less commonly can be temporary (such as in McArdle disease),[3] or resolve over time but reoccur later in life (such as in Bethlem myopathy 1).[4]
It is usually in response to prolonged hypertonic spasticity in a concentrated muscle area, such as is seen in the tightest muscles of people with conditions like spastic cerebral palsy, but can also be due to the congenital abnormal development of muscles and connective tissue in the womb.
Contractures develop usually when normally elastic tissues such as muscles or tendons are replaced by inelastic tissues (fibrosis). This results in the shortening and hardening of these tissues, ultimately causing rigidity, joint deformities and a total loss of movement around the joint.
Most of the physical therapy, occupational therapy and other exercise regimens targeted towards people with spasticity focuses on trying to prevent contractures from happening in the first place. However, research on sustained traction of connective tissue in approaches such as adaptive yoga has demonstrated that contracture can be reduced,[5] at the same time that tendency toward spasticity is addressed.
- ^ Clavet H, Hébert PC, Fergusson D, Doucette S, Trudel G (March 2008). "Joint contracture following prolonged stay in the intensive care unit". CMAJ. 178 (6): 691–7. doi:10.1503/cmaj.071056. PMC 2263098. PMID 18332384.
- ^ "Definition of contracture". www.cancer.gov. 2011-02-02. Retrieved 2023-05-06.
- ^ Lucia, Alejandro; Martinuzzi, Andrea; Nogales-Gadea, Gisela; Quinlivan, Ros; Reason, Stacey; International Association for Muscle Glycogen Storage Disease study group (December 2021). "Clinical practice guidelines for glycogen storage disease V & VII (McArdle disease and Tarui disease) from an international study group". Neuromuscular Disorders. 31 (12): 1296–1310. doi:10.1016/j.nmd.2021.10.006. ISSN 1873-2364. PMID 34848128. S2CID 240123241.
- ^ Bönnemann, Carsten G. (2011-06-21). "The collagen VI-related myopathies: muscle meets its matrix". Nature Reviews. Neurology. 7 (7): 379–390. doi:10.1038/nrneurol.2011.81. ISSN 1759-4758. PMC 5210181. PMID 21691338.
- ^ Nambi, Gopal S & Amisha Atul Kumar Shah (2013). "Additional effect of iyengar yoga and EMG biofeedback on pain and functional disability in chronic unilateral knee osteoarthritis". International Journal of Yoga. 6 (2): 123–127. doi:10.4103/0973-6131.113413. PMC 3734638. PMID 23930031.