| Diffuse large B cell lymphoma | |
|---|---|
| Other names | DLBCL or DLBL |
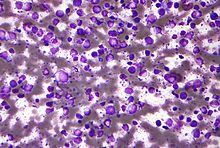 | |
| Micrograph (Field stain) of a diffuse large B cell lymphoma. | |
| Specialty | Hematology, oncology, dermatology |
Diffuse large B-cell lymphoma (DLBCL) is a cancer of B cells, a type of lymphocyte that is responsible for producing antibodies. It is the most common form of non-Hodgkin lymphoma among adults,[1] with an annual incidence of 7–8 cases per 100,000 people per year in the US and UK.[2][3] This cancer occurs primarily in older individuals, with a median age of diagnosis at ~70 years,[3] although it can occur in young adults and, in rare cases, children.[4] DLBCL can arise in virtually any part of the body and, depending on various factors, is often a very aggressive malignancy.[5] The first sign of this illness is typically the observation of a rapidly growing mass or tissue infiltration that is sometimes associated with systemic B symptoms, e.g. fever, weight loss, and night sweats.[6]
The causes of diffuse large B-cell lymphoma are not well understood. Usually DLBCL arises from normal B cells, but it can also represent a malignant transformation of other types of lymphoma (particularly marginal zone lymphomas[7]) or, in rare cases termed Richter's transformation, chronic lymphocytic leukemia.[8] An underlying immunodeficiency is a significant risk factor for development of the disease.[9] Infections with the Epstein–Barr virus (EBV),[10][11] Kaposi's sarcoma-associated herpesvirus,[12][13] human immunodeficiency virus (i.e. HIV),[12] and the Helicobacter pylori bacterium[7] are also associated with the development of certain subtypes of diffuse large B-cell lymphoma. However, most cases of this disease are associated with the unexplained step-wise acquisition of increasing numbers of gene mutations and changes in gene expression that occur in, and progressively promote the malignant behavior of, certain B-cell types.[14]
Diagnosis of DLBCL is made by removing a portion of the tumor through a biopsy, and then examining this tissue using a microscope. Usually a hematopathologist makes this diagnosis.[15] Numerous subtypes of DLBCL have been identified which differ in their clinical presentations, biopsy findings, aggressive characteristics, prognoses, and recommended treatments.[16] However, the usual treatment for most subtypes of DLBCL is chemotherapy combined with a monoclonal antibody drug that targets the disease's cancerous B-cells, usually rituximab.[17] Through these treatments, more than half of all patients with DLBCL can be cured;[18] the overall cure rate for older adults is less than this but their five-year survival rate has been around 58%.[19]
- ^ Cite error: The named reference
Blood1997was invoked but never defined (see the help page). - ^ Cite error: The named reference
Morton2006was invoked but never defined (see the help page). - ^ a b Cite error: The named reference
Smith2011was invoked but never defined (see the help page). - ^ Cite error: The named reference
Smith2010was invoked but never defined (see the help page). - ^ Cite error: The named reference
Kumar2009was invoked but never defined (see the help page). - ^ Cite error: The named reference
UpToDateEpi2012was invoked but never defined (see the help page). - ^ a b Casulo C, Friedberg J (2017). "Transformation of marginal zone lymphoma (and association with other lymphomas)". Best Practice & Research. Clinical Haematology. 30 (1–2): 131–138. doi:10.1016/j.beha.2016.08.029. PMID 28288708.
- ^ Abuelgasim KA, Rehan H, Alsubaie M, Al Atwi N, Al Balwi M, Alshieban S, Almughairi A (March 2018). "Coexistence of chronic myeloid leukemia and diffuse large B-cell lymphoma with antecedent chronic lymphocytic leukemia: a case report and review of the literature". Journal of Medical Case Reports. 12 (1): 64. doi:10.1186/s13256-018-1612-4. PMC 5845776. PMID 29524963.
- ^ Swerdlow et al. 2008, p. 233.
- ^ Castillo JJ, Beltran BE, Miranda RN, Young KH, Chavez JC, Sotomayor EM (July 2018). "EBV-positive diffuse large B-cell lymphoma, not otherwise specified: 2018 update on diagnosis, risk-stratification and management". American Journal of Hematology. 93 (7): 953–962. doi:10.1002/ajh.25112. hdl:20.500.12727/6261. PMID 29984868.
- ^ Nicolae A, Pittaluga S, Abdullah S, Steinberg SM, Pham TA, Davies-Hill T, Xi L, Raffeld M, Jaffe ES (August 2015). "EBV-positive large B-cell lymphomas in young patients: a nodal lymphoma with evidence for a tolerogenic immune environment". Blood. 126 (7): 863–72. doi:10.1182/blood-2015-02-630632. PMC 4536540. PMID 25999451.
- ^ a b Sukswai N, Lyapichev K, Khoury JD, Medeiros LJ (November 2019). "Diffuse large B-cell lymphoma variants: an update". Pathology. 52 (1): 53–67. doi:10.1016/j.pathol.2019.08.013. PMID 31735345. S2CID 208142227.
- ^ Shimada K, Hayakawa F, Kiyoi H (November 2018). "Biology and management of primary effusion lymphoma". Blood. 132 (18): 1879–1888. doi:10.1182/blood-2018-03-791426. PMID 30154110.
- ^ Liu Y, Barta SK (May 2019). "Diffuse large B-cell lymphoma: 2019 update on diagnosis, risk stratification, and treatment". American Journal of Hematology. 94 (5): 604–616. doi:10.1002/ajh.25460. PMID 30859597.
- ^ Goldman & Schafer 2012, p. 1222.
- ^ Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, Advani R, Ghielmini M, Salles GA, Zelenetz AD, Jaffe ES (May 2016). "The 2016 revision of the World Health Organization classification of lymphoid neoplasms". Blood. 127 (20): 2375–90. doi:10.1182/blood-2016-01-643569. PMC 4874220. PMID 26980727.
- ^ Goldman & Schafer 2012, p. 1225.
- ^ Cite error: The named reference
Akyurek2011was invoked but never defined (see the help page). - ^ Cite error: The named reference
Feugier2005was invoked but never defined (see the help page).