| Mycosis | |
|---|---|
| Other names | Mycoses,[1] fungal disease,[2] fungal infection[3] ICD-10CM codes: Mycoses B35-B49 [4] |
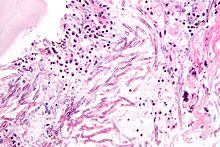 | |
| Micrograph showing a mycosis (aspergillosis). The Aspergillus (which is spaghetti-like) is seen in the center and surrounded by inflammatory cells and necrotic debris. H&E stain. | |
| Specialty | Infectious Diseases[5] |
| Types | Systemic, superficial, subcutaneous[3] |
| Causes | Pathogenic fungus: dermatophytes, yeasts, molds[6][7] |
| Risk factors | Immunodeficiency, cancer treatment, large surface area wounds/burns,[8][9] organ transplant,[6] COVID-19,[10] tuberculosis |
| Diagnostic method | Based on symptoms, culture, microscopic examination[6] |
| Treatment | Antifungals[3] |
| Frequency | Common[11] |
| Deaths | 1.7 million (2020)[12] |
Fungal infection, also known as mycosis, is a disease caused by fungi.[5][13] Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic.[3][6] Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor.[7] Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin.[1][7] Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis.[3] Signs and symptoms range widely.[3] There is usually a rash with superficial infection.[2] Fungal infection within the skin or under the skin may present with a lump and skin changes.[3] Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.[2]
Fungi are everywhere, but only some cause disease.[13] Fungal infection occurs after spores are either breathed in, come into contact with skin or enter the body through the skin such as via a cut, wound or injection.[3] It is more likely to occur in people with a weak immune system.[14] This includes people with illnesses such as HIV/AIDS, and people taking medicines such as steroids or cancer treatments.[14] Fungi that cause infections in people include yeasts, molds and fungi that are able to exist as both a mold and yeast.[3] The yeast Candida albicans can live in people without producing symptoms, and is able to cause both superficial mild candidiasis in healthy people, such as oral thrush or vaginal yeast infection, and severe systemic candidiasis in those who cannot fight infection themselves.[3]
Diagnosis is generally based on signs and symptoms, microscopy, culture, sometimes requiring a biopsy and the aid of medical imaging.[6] Some superficial fungal infections of the skin can appear similar to other skin conditions such as eczema and lichen planus.[7] Treatment is generally performed using antifungal medicines, usually in the form of a cream or by mouth or injection, depending on the specific infection and its extent.[15] Some require surgically cutting out infected tissue.[3]
Fungal infections have a world-wide distribution and are common, affecting more than one billion people every year.[11] An estimated 1.7 million deaths from fungal disease were reported in 2020.[12] Several, including sporotrichosis, chromoblastomycosis and mycetoma are neglected.[16]
A wide range of fungal infections occur in other animals, and some can be transmitted from animals to people.[17]
- ^ a b Johnstone RB (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. pp. 438–465. ISBN 978-0-7020-6830-0.
- ^ a b c "Fungal Diseases Homepage | CDC". www.cdc.gov. 29 March 2021. Retrieved 17 June 2021.
- ^ a b c d e f g h i j k Barlow G, Irving WL, Moss PJ (2020). "20. Infectious diseases". In Feather A, Randall D, Waterhouse M (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. pp. 559–563. ISBN 978-0-7020-7870-5.
- ^ ICD-10CM. mycoses B35-B49.
{{cite book}}: CS1 maint: numeric names: authors list (link) - ^ a b "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 25 May 2021.
- ^ a b c d e Willinger B (2019). "1. What is the target? Clinical mycology and diagnostics". In Presterl E (ed.). Clinically Relevant Mycoses: A Practical Approach. Germany: Springer. pp. 3–19. ISBN 978-3-319-92299-7.
- ^ a b c d Kutzner H, Kempf W, Feit J, Sangueza O (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. pp. 77–108. ISBN 978-1-119-64706-5.
- ^ Struck MF, Gille J (September 2013). "Fungal infections in burns: a comprehensive review". Annals of Burns and Fire Disasters. 26 (3): 147–153. PMC 3917146. PMID 24563641.
- ^ Kalan L, Grice EA (July 2018). "Fungi in the Wound Microbiome". Advances in Wound Care. 7 (7): 247–255. doi:10.1089/wound.2017.0756. PMC 6032664. PMID 29984114.
- ^ Cite error: The named reference
CDCFwas invoked but never defined (see the help page). - ^ a b Cite error: The named reference
Rai2020was invoked but never defined (see the help page). - ^ a b Kainz K, Bauer MA, Madeo F, Carmona-Gutierrez D (June 2020). "Fungal infections in humans: the silent crisis". Microbial Cell. 7 (6): 143–145. doi:10.15698/mic2020.06.718. PMC 7278517. PMID 32548176.
- ^ a b Richardson MD, Warnock DW (2012). "1. Introduction". Fungal Infection: Diagnosis and Management (4th ed.). John Wiley & Sons. pp. 1–7. ISBN 978-1-4051-7056-7.
- ^ a b Cite error: The named reference
CDCwhowas invoked but never defined (see the help page). - ^ Cite error: The named reference
Presterl3was invoked but never defined (see the help page). - ^ Queiroz-Telles F, Fahal AH, Falci DR, Caceres DH, Chiller T, Pasqualotto AC (November 2017). "Neglected endemic mycoses". The Lancet. Infectious Diseases. 17 (11): e367–e377. doi:10.1016/S1473-3099(17)30306-7. PMID 28774696.
- ^ Seyedmousavi S, Bosco SM, de Hoog S, Ebel F, Elad D, Gomes RR, et al. (April 2018). "Fungal infections in animals: a patchwork of different situations". Medical Mycology. 56 (suppl_1): 165–187. doi:10.1093/mmy/myx104. PMC 6251577. PMID 29538732.