| Idiopathic pulmonary fibrosis | |
|---|---|
| Other names | Fibrosing alveolitis, cryptogenic fibrosing alveolitis, diffuse fibrosing alveolitis, usual interstitial pneumonitis, diffuse interstitial pneumonitis |
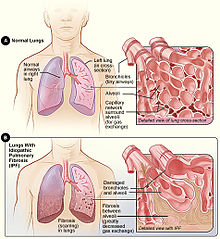 | |
| Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed view of the lung's airways and air sacs in cross-section. Figure B shows fibrosis (scarring) in the lungs. The inset image shows a detailed view of the fibrosis and how it damages the airways and air sacs.[1] | |
| Specialty | Pulmonology |
| Symptoms | Shortness of breath, dry coughing[1] |
| Complications | Pulmonary hypertension, heart failure, pneumonia, pulmonary embolism[1] |
| Usual onset | Gradual[1] |
| Causes | Unknown[2] |
| Risk factors | Cigarette smoking, certain viral infections, family history[1] |
| Diagnostic method | CT scan, lung biopsy[3] |
| Differential diagnosis | Sarcoidosis, other interstitial lung diseases, hypersensitivity pneumonitis[4] |
| Treatment | Pulmonary rehabilitation, supplemental oxygen, lung transplantation[1] |
| Medication | Pirfenidone, nintedanib[2] |
| Prognosis | Life expectancy ~ 4 years[1] |
| Frequency | 12 per 100,000 people per year[4] |
Idiopathic pulmonary fibrosis (IPF) synonymous with cryptogenic fibrosing alveolitis[5] is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic pulmonary fibrosis characterized by a progressive and irreversible decline in lung function.[6][3][4]
The tissue in the lungs becomes thick and stiff, which affects the tissue that surrounds the air sacs in the lungs.[7] Symptoms typically include gradual onset of shortness of breath and a dry cough.[1] Other changes may include feeling tired, and clubbing abnormally large and dome shaped finger and toenails.[1] Complications may include pulmonary hypertension, heart failure, pneumonia or pulmonary embolism.[1]
The cause is unknown, hence the term idiopathic.[2] Risk factors include cigarette smoking, acid reflux disease (GERD), certain viral infections, and genetic predisposition.[1] The underlying mechanism involves scarring of the lungs.[1] Diagnosis requires ruling out other potential causes.[3] It may be supported by a high resolution CT scan or lung biopsy which show usual interstitial pneumonia.[3] It is a type of interstitial lung disease.[3]
People often benefit from pulmonary rehabilitation and supplemental oxygen.[1] Certain medications like pirfenidone (Esbriet) or nintedanib (Ofev) may slow the progression of the disease.[2] Lung transplantation may also be an option.[1]
About 5 million people are affected globally.[8] The disease newly occurs in about 12 per 100,000 people per year.[4] Those in their 60s and 70s are most commonly affected.[4] Males are affected more often than females.[4] Average life expectancy following diagnosis is about four years.[1] Updated international guidelines were published in 2022, which some simplification in diagnosis and the removal of antacids as a possible adjunct therapy.[9]
- ^ a b c d e f g h i j k l m n o "Idiopathic Pulmonary Fibrosis". NHLBI. Retrieved 21 January 2018.
- ^ a b c d Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. (July 2015). "An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline". American Journal of Respiratory and Critical Care Medicine. 192 (2): e3–19. doi:10.1164/rccm.201506-1063ST. PMID 26177183.
- ^ a b c d e Raghu G, Collard HR, Egan JJ, et al. (2011). "An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management". American Journal of Respiratory and Critical Care Medicine. 183 (6): 788–824. doi:10.1164/rccm.2009-040GL. PMC 5450933. PMID 21471066.
- ^ a b c d e f Ferri FF (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 691. ISBN 9780323529570.
- ^ "Idiopathic pulmonary fibrosis | Information for the public | Idiopathic pulmonary fibrosis in adults: diagnosis and management | Guidance | NICE". www.nice.org.uk. 12 June 2013. Retrieved 15 June 2024.
- ^ Todd, Nevins W.; Luzina, Irina G.; Atamas, Sergei P. (2012). "Molecular and cellular mechanisms of pulmonary fibrosis". Fibrogenesis & Tissue Repair. 5 (1): 11. doi:10.1186/1755-1536-5-11. PMC 3443459. PMID 22824096.
- ^ "Idiopathic Pulmonary Fibrosis". NHLBI, NIH. Retrieved 5 December 2020.
- ^ Meltzer EB, Noble PW (2008). "Idiopathic pulmonary fibrosis". Orphanet Journal of Rare Diseases. 3 (1): 8. doi:10.1186/1750-1172-3-8. PMC 2330030. PMID 18366757.
- ^ Raghu, Ganesh; Remy-Jardin, Martine; Richeldi, Luca; Thomson, Carey C.; Inoue, Yoshikazu; Johkoh, Takeshi; Kreuter, Michael; Lynch, David A.; Maher, Toby M.; Martinez, Fernando J.; Molina-Molina, Maria; Myers, Jeffrey L.; Nicholson, Andrew G.; Ryerson, Christopher J.; Strek, Mary E. (1 May 2022). "Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline". American Journal of Respiratory and Critical Care Medicine. 205 (9): e18–e47. doi:10.1164/rccm.202202-0399ST. ISSN 1073-449X. PMC 9851481. PMID 35486072. S2CID 248432749.