| Insulitis | |
|---|---|
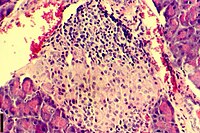 | |
| A histological image of an inflammatory infiltration of the islets of Langerhans of the pancreas | |
| Pronunciation | |
| Specialty | Endocrinology |
| Complications | Can lead to loss of beta cell function and can lead to type 1 diabetes[1] |
| Causes | Immune cell infiltration in islets of langerhans[2] |
| Management | islet cell transplantation[3] |
| Frequency | Found in 19% of people with T1D and 28% of people with T2D[2] |
Insulitis is an inflammation of the islets of Langerhans, a collection of endocrine tissue located in the pancreas that helps regulate glucose levels, and is classified by specific targeting of immune cell (T and B lymphocytes, macrophages and dendritic cells) infiltration in the islets of Langerhans.[4][5][6][7] This immune cell infiltration can result in the destruction of insulin-producing beta cells of the islets, which plays a major role in the pathogenesis, the disease development, of type 1 and type 2 diabetes. Insulitis is present in 19% of individuals with type 1 diabetes and 28% of individuals with type 2 diabetes.[1][8][9] It is known that genetic and environmental factors contribute to insulitis initiation, however, the exact process that causes it is unknown.[10] Insulitis is often studied using the non-obese diabetic (NOD) mouse model of type 1 diabetes. The chemokine family of proteins may play a key role in promoting leukocytic infiltration into the pancreas prior to pancreatic beta-cell destruction.[11]
- ^ a b In’t Veld, P. (2014). Insulitis in human type 1 diabetes: a comparison between patients and animal models. Semin Immunopathol 36, 569–579. https://doi.org/10.1007/s00281-014-0438-4
- ^ a b Cite error: The named reference
:5was invoked but never defined (see the help page). - ^ Cite error: The named reference
:10was invoked but never defined (see the help page). - ^ Campbell-Thompson ML, Atkinson MA, Butler AE, Chapman NM, Frisk G, Gianani R, Giepmans BN, von Herrath MG, Hyöty H, Kay TW, Korsgren O, Morgan NG, Powers AC, Pugliese A, Richardson SJ, Rowe PA, Tracy S, In't Veld PA (Nov 2013). "The diagnosis of insulitis in human type 1 diabetes". Diabetologia. 56 (11): 2541–2543. doi:10.1007/s00125-013-3043-5. PMID 24006089.
- ^ Campbell-Thompson M; Fu Ann; Wasserfall Clive; Kaddis John; Schatz Desmond; Pugliese Alberto; Atkinson Mark (Nov 2015). "Insulitis and beta cell mass in the natural history of type 1 diabetes". Diabetes. 65 (3): 719–731. doi:10.2337/db15-0779. PMC 4764143. PMID 26581594.
- ^ Rodriguez-Calvo T, Ekwall O, Amirian N, Zapardiel-Gonzalo J, von Herrath MG (2014). "Increased Immune Cell Infiltration of the Exocrine Pancreas: A Possible Contribution to the Pathogenesis of Type 1 Diabetes". Diabetes. 63 (11): 3880–3890. doi:10.2337/db14-0549. PMC 4207385. PMID 24947367.
- ^ Campbell-Thompson M, Rodriguez-Calvo R, Battaglia M (Oct 2015). "Abnormalities of the exocrine pancreas in type 1 diabetes". Curr Diab Rep. 15 (10): 79. doi:10.1007/s11892-015-0653-y. PMC 5072278. PMID 26318606.
- ^ Lundberg, M., Seiron, P., Ingvast, S., Korsgren, O., & Skog, O. (2017). Insulitis in human diabetes: a histological evaluation of donor pancreases. Diabetologia, 60(2), 346–353. https://doi.org/10.1007/s00125-016-4140-z
- ^ Haschek, W. M., Rousseaux, C. G., Wallig, M. A. (Eds.). (2013). Haschek and Rousseaux's Handbook of Toxicologic Pathology. Elsevier Inc. https://doi.org/10.1016/C2010-1-67850-9
- ^ Grönholm, J., & Lenardo, M. J. (2015). Novel diagnostic and therapeutic approaches for autoimmune diabetes--a prime time to treat insulitis as a disease. Clinical immunology (Orlando, Fla.), 156(2), 109–118. https://doi.org/10.1016/j.clim.2014.11.007
- ^ Burke SJ, Collier JJ (May 2015). "Transcriptional regulation of chemokine genes: a link to pancreatic islet inflammation?". Biomolecules. 5 (2): 1020–34. doi:10.3390/biom5021020. PMC 4496708. PMID 26018641.