| Metabolic acidosis | |
|---|---|
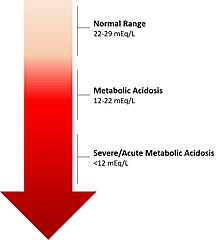 | |
| The calculated level of bicarbonate in the blood (HCO3−) reflects the severity of acidosis. | |
| Specialty | Nephrology |
| Complications | Acute: poor morbidity and mortality outcomes; Chronic: adverse outcomes on kidney function, musculoskeletal system, possible cardiovascular effects |
| Types | Acute Metabolic Acidosis Chronic Metabolic Acidosis |
| Causes | Acute: Excessive amounts of organic acids; Chronic: Impaired kidney function |
| Diagnostic method | Level of bicarbonate (HCO3-) in the blood |
| Treatment | Acute: Mitigation of the underlying cause for the metabolic problem, such as administration of insulin in cases of diabetic ketoacidosis or restoration of effective circulating intravascular volume in cases of lactic acidosis. The administration of IV bicarbonate, although intellectually appealing, is rarely indicated or administered Chronic: Diet rich in fruits and vegetables, oral alkali therapy[1] |
| Frequency | Acute: Most often presented during critical illnesses, and hospitalizations: incidence ranging 14–42%.[2][3] Chronic: Highly prevalent in people with Chronic Kidney Disease: 9.4% CKD Stage 3a; 18.1% CKD Stage 3b; 31.5% CKD Stage 4 and 5 [4] |
Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids.[5] Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35.[6] Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.
Acute metabolic acidosis, lasting from minutes to several days, often occurs during serious illnesses or hospitalizations, and is generally caused when the body produces an excess amount of organic acids (ketoacids in ketoacidosis, or lactic acid in lactic acidosis). A state of chronic metabolic acidosis, lasting several weeks to years, can be the result of impaired kidney function (chronic kidney disease) and/or bicarbonate wasting. The adverse effects of acute versus chronic metabolic acidosis also differ, with acute metabolic acidosis impacting the cardiovascular system in hospital settings, and chronic metabolic acidosis affecting muscles, bones, kidney and cardiovascular health.[7]
- ^ Navaneethan, Sankar D.; Shao, Jun; Buysse, Jerry; Bushinsky, David A. (5 July 2019). "Effects of Treatment of Metabolic Acidosis in CKD: A Systematic Review and Meta-Analysis". Clinical Journal of the American Society of Nephrology. 14 (7): 1011–1020. doi:10.2215/CJN.13091118. PMC 6625635. PMID 31196951.
- ^ Kraut, Jeffrey A.; Madias, Nicolaos E. (4 September 2012). "Treatment of acute metabolic acidosis: a pathophysiologic approach". Nature Reviews Nephrology. 8 (10): 589–601. doi:10.1038/nrneph.2012.186. PMID 22945490. S2CID 34657707.
- ^ Jung, Boris; Rimmele, Thomas; Le Goff, Charlotte; Chanques, Gérald; Corne, Philippe; Jonquet, Olivier; Muller, Laurent; Lefrant, Jean-Yves; Guervilly, Christophe; Papazian, Laurent; Allaouchiche, Bernard; Jaber, Samir (2011). "Severe metabolic or mixed acidemia on intensive care unit admission: incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study". Critical Care. 15 (5): R238. doi:10.1186/cc10487. PMC 3334789. PMID 21995879.
- ^ Inker, Lesley A.; Coresh, Josef; Levey, Andrew S.; Tonelli, Marcello; Muntner, Paul (1 December 2011). "Estimated GFR, Albuminuria, and Complications of Chronic Kidney Disease". Journal of the American Society of Nephrology. 22 (12): 2322–2331. doi:10.1681/ASN.2010111181. PMC 3279937. PMID 21965377.
- ^ Emmett, Michael; Szerlip, Harold. "Approach to the adult with metabolic acidosis".
- ^ Costanzo, Linda (2010). Physiology. Philadelphia, Pennsylvania: Elsevier. ISBN 978-1-4160-6216-5.
- ^ Kraut, Jeffrey A.; Madias, Nicolaos E. (2010-05-01). "Metabolic acidosis: pathophysiology, diagnosis and management". Nature Reviews Nephrology. 6 (5): 274–285. doi:10.1038/nrneph.2010.33. ISSN 1759-5061. PMID 20308999. S2CID 205512465.