| Neutropenia | |
|---|---|
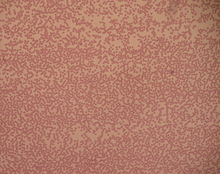 | |
| Blood film with a striking absence of neutrophils, leaving only red blood cells and platelets | |
| Specialty | Infectious disease, Hematology |
| Causes | Aplastic anemia, Glycogen storage disease, Cohen syndrome,[1][2] gene mutations |
| Diagnostic method | CBC[3] |
| Treatment | Antibiotics, Splenectomy if needed,[3] G-CSF |
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood.[4] Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood.[5] People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening (neutropenic sepsis).[6]
Neutropenia can be divided into congenital and acquired, with severe congenital neutropenia (SCN) and cyclic neutropenia (CyN) being autosomal dominant and mostly caused by heterozygous mutations in the ELANE gene (neutrophil elastase).[7] Neutropenia can be acute (temporary) or chronic (long lasting). The term is sometimes used interchangeably with "leukopenia" ("deficit in the number of white blood cells").[8]
Decreased production of neutrophils is associated with deficiencies of vitamin B12 and folic acid, aplastic anemia, tumors, drugs, metabolic disease, nutritional deficiencies (including minerals such as copper), and immune mechanisms. In general, the most common oral manifestations of neutropenia include ulcer, gingivitis, and periodontitis. Agranulocytosis can be presented as whitish or greyish necrotic ulcer in the oral cavity, without any sign of inflammation. Acquired agranulocytosis is much more common than the congenital form. The common causes of acquired agranulocytosis including drugs (non-steroidal anti-inflammatory drugs, antiepileptics, antithyroid, and antibiotics) and viral infection. Agranulocytosis has a mortality rate of 7–10%. To manage this, the application of granulocyte colony stimulating factor (G-CSF) or granulocyte transfusion and the use of broad-spectrum antibiotics to protect against bacterial infections are recommended.[9]
- ^ Cite error: The named reference
Ohls2012was invoked but never defined (see the help page). - ^ Cite error: The named reference
evalwas invoked but never defined (see the help page). - ^ a b Cite error: The named reference
medwas invoked but never defined (see the help page). - ^ "Neutropenia". National Center for Biotechnology, National Library of Medicine. Retrieved 8 December 2015.
- ^ "Neutrophils". National Center for Biotechnology, National Library of Medicine. Retrieved 8 December 2015.
- ^ Cite error: The named reference
FredricksFung2015was invoked but never defined (see the help page). - ^ Horwitz MS, Corey SJ, Grimes HL, Tidwell T (February 2013). "ELANE mutations in cyclic and severe congenital neutropenia: genetics and pathophysiology". Hematology/Oncology Clinics of North America. 27 (1): 19–41, vii. doi:10.1016/j.hoc.2012.10.004. PMC 3559001. PMID 23351986.
- ^ Boxer LA (8 December 2012). "How to approach neutropenia". Hematology. American Society of Hematology. Education Program. 2012 (1): 174–82. doi:10.1182/asheducation.v2012.1.174.3798251. PMID 23233578.
- ^ Nakai, Yukie; Ishihara, Chikako; Ogata, Sagiri; Shimono, Tsutomu (July 2003). "Oral manifestations of cyclic neutropenia in a Japanese child: case report with a 5-year follow-up" (PDF). Pediatric Dentistry. 25 (4): 383–8. PMID 13678105. S2CID 24909338.