| |||
| Names | |||
|---|---|---|---|
| Pronunciation | /ˈnaɪəsɪn/ | ||
| Preferred IUPAC name
Pyridine-3-carboxylic acid[1] | |||
Other names
| |||
| Identifiers | |||
3D model (JSmol)
|
|||
| 3DMet | |||
| 109591 | |||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| ECHA InfoCard | 100.000.401 | ||
| EC Number |
| ||
| 3340 | |||
| KEGG | |||
| MeSH | Niacin | ||
PubChem CID
|
|||
| RTECS number |
| ||
| UNII | |||
CompTox Dashboard (EPA)
|
|||
| |||
| |||
| Properties | |||
| C6H5NO2 | |||
| Molar mass | 123.111 g·mol−1 | ||
| Appearance | White, translucent crystals | ||
| Density | 1.473 g cm−3 | ||
| Melting point | 237 °C; 458 °F; 510 K | ||
| 18 g L−1 | |||
| log P | 0.219 | ||
| Acidity (pKa) | 2.0, 4.85 | ||
| Isoelectric point | 4.75 | ||
Refractive index (nD)
|
1.4936 | ||
| 0.1271305813 D[citation needed] | |||
| Thermochemistry | |||
Std enthalpy of
formation (ΔfH⦵298) |
−344.9 kJ mol−1 | ||
Std enthalpy of
combustion (ΔcH⦵298) |
−2.73083 MJ mol−1 | ||
| Pharmacology | |||
| C04AC01 (WHO) C10BA01 (WHO) C10AD02 (WHO) C10AD52 (WHO) | |||
| License data |
| ||
| Intramuscular, by mouth | |||
| Pharmacokinetics: | |||
| 20–45 min | |||
| Hazards | |||
| GHS labelling: | |||

| |||
| Warning | |||
| H319 | |||
| P264, P280, P305+P351+P338, P337+P313, P501 | |||
| NFPA 704 (fire diamond) | |||
| Flash point | 193 °C (379 °F; 466 K) | ||
| 365 °C (689 °F; 638 K) | |||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |||
| Clinical data | |
|---|---|
| Trade names | Niacor, Niaspan, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682518 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intramuscular, by mouth |
| Legal status | |
| Legal status |
|
| Identifiers | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.401 |
Niacin, also known as nicotinic acid, is an organic compound and a vitamer of vitamin B3, an essential human nutrient.[3] It is produced by plants and animals from the amino acid tryptophan.[4] Niacin is obtained in the diet from a variety of whole and processed foods, with highest contents in fortified packaged foods, meat, poultry, red fish such as tuna and salmon, lesser amounts in nuts, legumes and seeds.[3][5] Niacin as a dietary supplement is used to treat pellagra, a disease caused by niacin deficiency. Signs and symptoms of pellagra include skin and mouth lesions, anemia, headaches, and tiredness.[6] Many countries mandate its addition to wheat flour or other food grains, thereby reducing the risk of pellagra.[3][7]
The amide derivative nicotinamide (niacinamide) is a component of the coenzymes nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP+). Although niacin and nicotinamide are identical in their vitamin activity, nicotinamide does not have the same pharmacological, lipid-modifying effects or side effects as niacin, i.e., when niacin takes on the -amide group, it does not reduce cholesterol nor cause flushing.[8][9] Nicotinamide is recommended as a treatment for niacin deficiency because it can be administered in remedial amounts without causing the flushing, considered an adverse effect.[10]
Niacin is also a prescription medication.[11] Amounts far in excess of the recommended dietary intake for vitamin functions will lower blood triglycerides and low density lipoprotein cholesterol (LDL-C), and raise blood high density lipoprotein cholesterol (HDL-C, often referred to as "good" cholesterol). There are two forms: immediate-release and sustained-release niacin. Initial prescription amounts are 500 mg/day, increased over time until a therapeutic effect is achieved. Immediate-release doses can be as high as 3,000 mg/day; sustained-release as high as 2,000 mg/day.[11] Despite the proven lipid changes, niacin has not been found useful for decreasing the risk of cardiovascular disease in those already on a statin.[12] A 2010 review had concluded that niacin was effective as a mono-therapy,[13] but a 2017 review incorporating twice as many trials concluded that prescription niacin, while affecting lipid levels, did not reduce all-cause mortality, cardiovascular mortality, myocardial infarctions, nor fatal or non-fatal strokes.[14] Prescription niacin was shown to cause hepatotoxicity[15] and increase risk of type 2 diabetes.[16][17] Niacin prescriptions in the U.S. had peaked in 2009 at 9.4 million, declining to 800 thousand by 2020.[18]
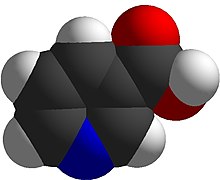
Niacin has the formula C
6H
5NO
2 and belongs to the group of the pyridinecarboxylic acids.[3] As the precursor for nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate, niacin is involved in DNA repair.[19]
- ^ "Chapter P-6. Applications to Specific Classes of Compounds". Nomenclature of Organic Chemistry : IUPAC Recommendations and Preferred Names 2013 (Blue Book). Cambridge: Royal Society of Chemistry. 2014. pp. 648–1047. doi:10.1039/9781849733069-00648. ISBN 978-0-85404-182-4.
- ^ "Niacin Use During Pregnancy". Drugs.com. 29 July 2019. Archived from the original on 5 August 2020. Retrieved 4 May 2020.
- ^ a b c d "Niacin". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis, OR. 8 October 2018. Archived from the original on 12 September 2019. Retrieved 16 September 2019.
- ^ Cite error: The named reference
DRItextwas invoked but never defined (see the help page). - ^ Cite error: The named reference
NIH Fact Sheetwas invoked but never defined (see the help page). - ^ Cite error: The named reference
Hegyi2004was invoked but never defined (see the help page). - ^ "Why fortify?". Food Fortification Initiative. 2017. Archived from the original on 4 April 2017. Retrieved 4 April 2017.
- ^ Jaconello P (October 1992). "Niacin versus niacinamide". CMAJ. 147 (7): 990. PMC 1336277. PMID 1393911.
- ^ Kirkland JB (May 2012). "Niacin requirements for genomic stability". Mutation Research. 733 (1–2): 14–20. Bibcode:2012MRFMM.733...14K. doi:10.1016/j.mrfmmm.2011.11.008. PMID 22138132. Archived from the original on 4 August 2020. Retrieved 3 July 2019.
- ^ Cite error: The named reference
Pellagra And Its Preventionwas invoked but never defined (see the help page). - ^ a b "Niacin". Drugs.com. 16 March 2019. Archived from the original on 9 June 2020. Retrieved 27 April 2020.
- ^ Cite error: The named reference
Kee2014was invoked but never defined (see the help page). - ^ Bruckert E, Labreuche J, Amarenco P (June 2010). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
- ^ Cite error: The named reference
Schand2017was invoked but never defined (see the help page). - ^ Cite error: The named reference
LiverTox2014was invoked but never defined (see the help page). - ^ Cite error: The named reference
Ong2014was invoked but never defined (see the help page). - ^ Cite error: The named reference
Goldie2016was invoked but never defined (see the help page). - ^ "Niacin - Drug Usage Statistics". ClinCalc. Archived from the original on 8 July 2020. Retrieved 7 October 2022.
- ^ Kennedy DO (January 2016). "B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review". Nutrients. 8 (2): 68. doi:10.3390/nu8020068. PMC 4772032. PMID 26828517.


