| Non-steroidal anti-inflammatory drug | |
|---|---|
| Drug class | |
 | |
| Class identifiers | |
| Pronunciation | /ˈɛnsɛd/ EN-sed |
| Synonyms | |
| Use | Pain,[1] fever,[1] inflammation,[1] antithrombosis[citation needed] |
| ATC code | M01A |
| Mechanism of action | Enzyme inhibitor |
| Biological target | COX-1 and COX-2 |
| Legal status | |
| In Wikidata | |
Non-steroidal anti-inflammatory drugs[1][3] (NSAID)[1] are members of a therapeutic drug class which reduces pain,[4] decreases inflammation, decreases fever,[1] and prevents blood clots. Side effects depend on the specific drug, its dose and duration of use, but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.[5][6]
The term non-steroidal, common from around 1960, distinguishes these drugs from corticosteroids, another class of anti-inflammatory drugs,[7] which during the 1950s had acquired a bad reputation due to overuse and side-effect problems after their introduction in 1948.[8][9][10]
NSAIDs work by inhibiting the activity of cyclooxygenase enzymes (the COX-1 and COX-2 isoenzymes). In cells, these enzymes are involved in the synthesis of key biological mediators, namely prostaglandins, which are involved in inflammation, and thromboxanes, which are involved in blood clotting.
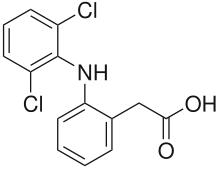
There are two general types of NSAIDs available: non-selective and COX-2 selective.[11] Most NSAIDs are non-selective, and inhibit the activity of both COX-1 and COX-2. These NSAIDs, while reducing inflammation, also inhibit platelet aggregation and increase the risk of gastrointestinal ulcers and bleeds.[11] COX-2 selective inhibitors have fewer gastrointestinal side effects, but promote thrombosis, and some of these agents substantially increase the risk of heart attack. As a result, certain COX-2 selective inhibitors—such as rofecoxib—are no longer used due to the high risk of undiagnosed vascular disease.[11] These differential effects are due to the different roles and tissue localisations of each COX isoenzyme.[11] By inhibiting physiological COX activity, NSAIDs may cause deleterious effects on kidney function,[12] and, perhaps as a result of water and sodium retention and decreases in renal blood flow, may lead to heart problems.[13] In addition, NSAIDs can blunt the production of erythropoietin, resulting in anaemia, since haemoglobin needs this hormone to be produced.
The most prominent NSAIDs are aspirin, ibuprofen, and naproxen; all available over the counter (OTC) in most countries.[14] Paracetamol (acetaminophen) is generally not considered an NSAID because it has only minor anti-inflammatory activity. Paracetamol treats pain mainly by blocking COX-2 and inhibiting endocannabinoid reuptake almost exclusively within the brain, and only minimally in the rest of the body.[15][16]
- ^ a b c d e f "non-steroidal anti-inflammatory drug". www.Lexico.com. Oxford English Dictionary. 2022. Archived from the original on 5 February 2022. Retrieved 4 February 2022.
- ^ a b Ghlichloo I, Gerriets V (1 May 2023), "Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31613522, archived from the original on 23 April 2024, retrieved 31 March 2024
- ^ "Non-steroidal anti-inflammatory drugs". BNF.NICE.org.uk. British National Formulary (BNF), National Institute for Health and Care Excellence (NICE). 2022. Retrieved 4 February 2022.
- ^ Mallinson TE (2 December 2017). "A review of ketorolac as a prehospital analgesic". Journal of Paramedic Practice. 9 (12): 522–526. doi:10.12968/jpar.2017.9.12.522. ISSN 1759-1376.
- ^ Bally M, Dendukuri N, Rich B, Nadeau L, Helin-Salmivaara A, Garbe E, et al. (May 2017). "Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data". The BMJ. 357: j1909. doi:10.1136/bmj.j1909. PMC 5423546. PMID 28487435.
- ^ Lanas A, Chan FK (August 2017). "Peptic ulcer disease". The Lancet. 390 (10094): 613–624. doi:10.1016/S0140-6736(16)32404-7. PMID 28242110. S2CID 4547048.
- ^ Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, et al. (August 2013). "A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy". Allergy, Asthma, and Clinical Immunology. 9 (1): 30. doi:10.1186/1710-1492-9-30. PMC 3765115. PMID 23947590.
- ^ Buer JK (October 2014). "Origins and impact of the term 'NSAID'". Inflammopharmacology. 22 (5): 263–267. doi:10.1007/s10787-014-0211-2. hdl:10852/45403. PMID 25064056. S2CID 16777111.
- ^ Case JP (2001). "Old and new drugs used in rheumatoid arthritis: a historical perspective. Part 1: the older drugs". American Journal of Therapeutics. 8 (2): 123–143. doi:10.1097/00045391-200103000-00007. PMID 11304666.
- ^ LeFanu J (2011). The Rise and Fall of Modern Medicine. Abacus. p. 34.
- ^ a b c d Day RO, Graham GG (2004). "The Vascular Effects of COX-2 selective inhibitors". Australian Prescriber. 27 (6): 142–145. doi:10.18773/austprescr.2004.119.
- ^ Brater DC, Harris C, Redfern JS, Gertz BJ (January 2001). "Renal effects of COX-2-selective inhibitors". American Journal of Nephrology. 21 (1): 1–15. doi:10.1159/000046212. PMID 11275626. S2CID 35586796.
- ^ Bleumink GS, Feenstra J, Sturkenboom MC, Stricker BH (2003). "Nonsteroidal anti-inflammatory drugs and heart failure". Drugs. 63 (6): 525–34. doi:10.2165/00003495-200363060-00001. PMID 12656651. S2CID 24128916.
- ^ Warden SJ (April 2010). "Prophylactic use of NSAIDs by athletes: a risk / benefit assessment". The Physician and Sportsmedicine. 38 (1): 132–8. doi:10.3810/psm.2010.04.1770. PMID 20424410. S2CID 44567896.
- ^ Hinz B, Cheremina O, Brune K (February 2008). "Acetaminophen (paracetamol) is a selective cyclooxygenase-2 inhibitor in man". FASEB Journal. 22 (2): 383–90. doi:10.1096/fj.07-8506com. PMID 17884974. S2CID 9633350.
- ^ Page CP, Curtis MJ, Sutter M, Walker M, Hoffman B (1998). Farmacología integrada (in Spanish). Elsevier España. ISBN 84-8174-340-2 – via Google Books.