| Primary aldosteronism | |
|---|---|
| Other names | Primary hyperaldosteronism, Conn's syndrome |
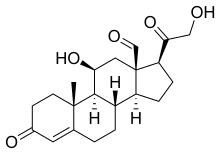 | |
| Aldosterone | |
| Specialty | Endocrinology |
| Symptoms | High blood pressure, poor vision, headaches, muscular weakness, muscle spasms[1][2] |
| Complications | Stroke, myocardial infarction, kidney failure, abnormal heart rhythms[3][4] |
| Usual onset | 30 to 50 years old[5] |
| Causes | Enlargement of both adrenal glands, adrenal adenoma, adrenal cancer, familial hyperaldosteronism[6][1] |
| Diagnostic method | Blood test for aldosterone-to-renin ratio[1] |
| Treatment | Surgery, spironolactone, eplerenone, low salt diet[1] |
| Frequency | 10% of people with high blood pressure[1] |
Primary aldosteronism (PA), also known as primary hyperaldosteronism, refers to the excess production of the hormone aldosterone from the adrenal glands, resulting in low renin levels and high blood pressure.[1] This abnormality is a paraneoplastic syndrome (i.e. caused by hyperplasia or tumors). About 35% of the cases are caused by a single aldosterone-secreting adenoma, a condition known as Conn's syndrome.[7][8]
Many patients experience fatigue, potassium deficiency and high blood pressure which may cause poor vision, confusion or headaches.[1][2] Symptoms may also include: muscular aches and weakness, muscle spasms, low back and flank pain from the kidneys, trembling, tingling sensations, dizziness/vertigo, nocturia and excessive urination.[1] Complications include cardiovascular disease such as stroke, myocardial infarction, kidney failure and abnormal heart rhythms.[3][4]
Primary hyperaldosteronism has a number of causes. About 33% of cases are due to an adrenal adenoma that produces aldosterone, and 66% of cases are due to an enlargement of both adrenal glands.[1] Other uncommon causes include adrenal cancer and an inherited disorder called familial hyperaldosteronism.[6] PA is under diagnosed; the Endocrine Society recommends screening people with high blood pressure who are at increased risk,[9] while others recommend screening all people with high blood pressure for the disease.[3] Screening is usually done by measuring the aldosterone-to-renin ratio in the blood (ARR) whilst off interfering medications and a serum potassium over 4, with further testing used to confirm positive results.[1] While low blood potassium is classically described in primary hyperaldosteronism, this is only present in about a quarter of people.[1] To determine the underlying cause, medical imaging is carried out.[1]
Some cases may be cured by removing the adenoma by surgery after localization with adrenal venous sampling (AVS).[1][10] A single adrenal gland may also be removed in cases where only one is enlarged.[4] In cases due to enlargement of both glands, treatment is typically with medications known as aldosterone antagonists such as spironolactone or eplerenone.[1] Other medications for high blood pressure and a low salt diet, e.g. DASH diet, may also be needed.[1][4] Some people with familial hyperaldosteronism may be treated with the steroid dexamethasone.[1]
Primary aldosteronism is present in about 10% of people with high blood pressure.[1] It occurs more often in women than men.[5] Often, it begins in those between 30 and 50 years of age.[5] Conn's syndrome is named after Jerome W. Conn (1907–1994), an American endocrinologist who first described adenomas as a cause of the condition in 1955.[11][12]
- ^ a b c d e f g h i j k l m n o p q Schirpenbach C, Reincke M (March 2007). "Primary aldosteronism: current knowledge and controversies in Conn's syndrome". Nature Clinical Practice. Endocrinology & Metabolism. 3 (3): 220–227. doi:10.1038/ncpendmet0430. PMID 17315030. S2CID 23220252.
- ^ a b "Primary hyperaldosteronism (Conn's syndrome or aldosterone-producing adrenal tumor)". Archived from the original on 19 April 2015. Retrieved 8 April 2015.
- ^ a b c Stowasser M, Taylor PJ, Pimenta E, Ahmed AH, Gordon RD (May 2010). "Laboratory investigation of primary aldosteronism". The Clinical Biochemist. Reviews. 31 (2): 39–56. PMC 2874431. PMID 20498828.
- ^ a b c d "Primary hyperaldosteronism (Conn's syndrome or aldosterone-producing adrenal tumor)". Archived from the original on 28 March 2015. Retrieved 8 April 2015.
- ^ a b c Hubbard JG, Inabnet WB, Heerden CY (2009). Endocrine surgery principles and practice. London: Springer. p. 367. ISBN 9781846288814. Archived from the original on 2016-06-30.
- ^ a b "Primary hyperaldosteronism (Conn's syndrome or aldosterone-producing adrenal tumor)". Archived from the original on 9 April 2015. Retrieved 8 April 2015.
- ^ Kumar V, Abbas AK, Aster JC, Turner JR, Perkins JA, Robbins SL, Cotran RS, eds. (2021). Robbins & Cotran Pathologic Basis of Disease (10th ed.). Philadelphia, PA: Elsevier. p. 1119. ISBN 978-0-323-53113-9.
- ^ Harrison's Principles of Internal Medicine (21st ed.). New York: McGraw Hill. 2022. pp. 2963–2965. ISBN 978-1-264-26850-4.
- ^ Cobb A, Aeddula NR (2023). "Primary Hyperaldosteronism". StatPearls. StatPearls Publishing. PMID 30969601.
- ^ Cusumano LR, Mathevosian S, Sweigert JK, Srinivasa RN, Luhar AP, Moriarty JM (January 2021). "Use of Bony Landmarks during Adrenal Venous Sampling to Guide Catheterization of the Left Adrenal Vein". The Arab Journal of Interventional Radiology. 5 (1): 25–29. doi:10.1055/s-0041-1730113. ISSN 2542-7075.
- ^ Conn JW, Louis LH (1955). "Primary aldosteronism: a new clinical entity". Transactions of the Association of American Physicians. 68: 215–31, discussion, 231–3. PMID 13299331.
- ^ Williams GH (2009). Textbook of nephro-endocrinology. Amsterdam: Academic. p. 372. ISBN 9780080920467. Archived from the original on 2016-06-30.