| Proliferative fasciitis and proliferative myositis | |
|---|---|
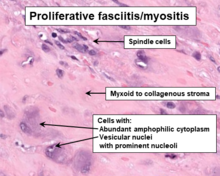 | |
| Histopathology of proliferative fasciitis or proliferative myositis | |
| Specialty | Dermatology, General surgery |
| Usual onset | Very rapid |
| Duration | Often regresses spontaneously within weeks of diagnosis |
| Treatment | symptomatic therapy, watchful waiting, surgical resection |
| Prognosis | Excellent |
| Frequency | Extremely rare |
Proliferative fasciitis and proliferative myositis (PF/PM) are rare benign soft tissue lesions (i.e. a damaged or unspecified abnormal change in a tissue) that increase in size over several weeks and often regress over the ensuing 1–3 months.[1] The lesions in PF/PM are typically obvious tumors or swellings. Historically, many studies had grouped the two descriptive forms of PF/PM as similar disorders with the exception that proliferative fasciitis occurs in subcutaneous tissues[2] while proliferative myositis occurs in muscle tissues.[3] In 2020, the World Health Organization agreed with this view and defined these lesions as virtually identical disorders termed proliferative fasciitis/proliferative myositis or proliferative fasciitis and proliferative myositis. The Organization also classified them as one of the various forms of the fibroblastic and myofibroblastic tumors.[4]
PF/PM lesions have been regarded as a tissue's self-limiting reaction to an injury or unidentified insult rather than an abnormal growth of a clone of neoplastic cells, that is, as a group of cells which share a common ancestry, have similar abnormalities in the expression and/or content of their genetic material, and often grow in a continuous and unrestrained manner.[5] However, a recent study has found a common genetic abnormality in some of the cells in most PF/FM tumors. This suggests that PF/PM are, in at least most cases, neoplastic but nonetheless self-limiting and/or spontaneously reversing disorders. That is, they are examples of "transient neoplasms." In all events, PF/PM lesions are benign tumor growths that do not metastasize.[6]
PF/PM lesions may grow at alarming rates,[3] exhibit abnormal histopathologies (e.g. high numbers and overcrowding of cells), and have other elements that are suggestive of a malignancy.[7] Consequently, they have been mistakenly diagnosed as undifferentiated pleomorphic sarcoma (also termed malignant fibrous histiocytoma), rhabdomyosarcoma,[1] or other types of sarcoma[8] and treated unnecessarily with aggressive measures used for such malignancies, e.g. wide surgical resection, radiation therapy, and chemotherapy.[1][9] The majority of PF/PM lesions are successfully treated with strictly conservative and supportive measures.[6]
- ^ a b c Nishi TM, Yamashita S, Hirakawa YN, Katsuki NE, Tago M, Yamashita SI (September 2019). "Proliferative Fasciitis/Myositis Involving the Facial Muscles Including the Masseter Muscle: A Rare Cause of Trismus". The American Journal of Case Reports. 20: 1411–1417. doi:10.12659/AJCR.917193. PMC 6777384. PMID 31551403.
- ^ Porrino J, Al-Dasuqi K, Irshaid L, Wang A, Kani K, Haims A, Maloney E (June 2021). "Update of pediatric soft tissue tumors with review of conventional MRI appearance-part 1: tumor-like lesions, adipocytic tumors, fibroblastic and myofibroblastic tumors, and perivascular tumors". Skeletal Radiology. 51 (3): 477–504. doi:10.1007/s00256-021-03836-2. PMID 34191084. S2CID 235678096.
- ^ a b Brooks JK, Scheper MA, Kramer RE, Papadimitriou JC, Sauk JJ, Nikitakis NG (April 2007). "Intraoral proliferative myositis: case report and literature review". Head & Neck. 29 (4): 416–20. doi:10.1002/hed.20530. PMID 17111425. S2CID 9698761.
- ^ Sbaraglia M, Bellan E, Dei Tos AP (April 2021). "The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives". Pathologica. 113 (2): 70–84. doi:10.32074/1591-951X-213. PMC 8167394. PMID 33179614.
- ^ Wong NL, Di F (December 2009). "Pseudosarcomatous fasciitis and myositis: diagnosis by fine-needle aspiration cytology". American Journal of Clinical Pathology. 132 (6): 857–65. doi:10.1309/AJCPLEPS44PJHDPP. PMID 19926576.
- ^ a b Makise N, Mori T, Motoi T, Shibahara J, Ushiku T, Yoshida A (May 2021). "Recurrent FOS rearrangement in proliferative fasciitis/proliferative myositis". Modern Pathology. 34 (5): 942–950. doi:10.1038/s41379-020-00725-2. PMID 33318581. S2CID 228627775.
- ^ Satish S, Shivalingaiah SC, Ravishankar S, Vimalambika MG (October 2012). "Fine needle aspiration cytology of pseudosarcomatous reactive lesions of soft tissues: A report of two cases". Journal of Cytology. 29 (4): 264–6. doi:10.4103/0970-9371.103949. PMC 3543599. PMID 23326034.
- ^ Gan S, Xie D, Dai H, Zhang Z, Di X, Li R, Guo L, Sun Y (2019). "Proliferative myositis and nodular fasciitis: a retrospective study with clinicopathologic and radiologic correlation". International Journal of Clinical and Experimental Pathology. 12 (12): 4319–4328. PMC 6949867. PMID 31933833.
- ^ Meis JM, Enzinger FM (April 1992). "Proliferative fasciitis and myositis of childhood". The American Journal of Surgical Pathology. 16 (4): 364–72. doi:10.1097/00000478-199204000-00005. PMID 1566969. S2CID 20591490.