| Pulmonary hypertension | |
|---|---|
| Other names | Ayerza syndrome[1] |
 | |
| Pulmonary hypertension | |
| Specialty | Pulmonology, cardiology |
| Symptoms | Chest pain, fatigue[2] |
| Usual onset | 20 to 60 years old[3] |
| Duration | Long term[4] |
| Causes | Unknown[4] |
| Risk factors | Family history, pulmonary embolism, HIV/AIDS, sickle cell disease, cocaine use, COPD, sleep apnea, living at high altitudes[5][3] |
| Diagnostic method | Following ruling out other potential causes[4] |
| Treatment | Supportive care, various medications, lung transplantation[4][6] |
| Medication | Epoprostenol, treprostinil, iloprost, bosentan, ambrisentan, macitentan, sildenafil[4] |
| Frequency | 1,000 new cases a year (US)[1] |
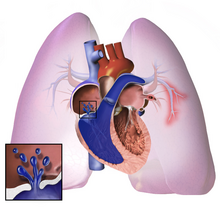
Pulmonary hypertension (PH or PHTN) is a condition of increased blood pressure in the arteries of the lungs.[7] Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat.[7][1] The condition may make it difficult to exercise.[7] Onset is typically gradual.[8] According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.
The cause is often unknown.[4] Risk factors include a family history, prior pulmonary embolism (blood clots in the lungs), HIV/AIDS, sickle cell disease, cocaine use, chronic obstructive pulmonary disease, sleep apnea, living at high altitudes, and problems with the mitral valve.[5][3] The underlying mechanism typically involves inflammation and subsequent remodeling of the arteries in the lungs.[5] Diagnosis involves first ruling out other potential causes.[4]
As of 2022[update] there was no cure for pulmonary hypertension,[6] although research to find a cure is ongoing. Treatment depends on the type of disease.[6] A number of supportive measures such as oxygen therapy, diuretics, and medications to inhibit blood clotting may be used.[4] Medications specifically used to treat pulmonary hypertension include epoprostenol, treprostinil, iloprost, bosentan, ambrisentan, macitentan, and sildenafil, tadalafil, selexipag, riociguat.[4] Lung transplantation may be an option in severe cases.[6]
The frequency of occurrence is estimated at 1,000 new cases per year in the United States.[3][1] Females are more often affected than males.[1] Onset is typically between 20 and 60 years of age.[3] Pulmonary hypertension was identified by Ernst von Romberg in 1891.[9][4]
- ^ a b c d e "Pulmonary arterial hypertension". Genetics Home Reference. January 2016. Archived from the original on 28 July 2017. Retrieved 30 July 2017.
- ^ Cite error: The named reference
www.nhlbi.nih.govwas invoked but never defined (see the help page). - ^ a b c d e "Who Is at Risk for Pulmonary Hypertension?". NHLBI – NIH. 2 August 2011. Archived from the original on 31 July 2017. Retrieved 30 July 2017.
- ^ a b c d e f g h i j Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RM, Brida M, et al. (October 2022). "2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension". European Heart Journal. 43 (38): 3618–3731. doi:10.1093/eurheartj/ehac237. PMID 36017548.
- ^ a b c "Causes and Risk Factors". Health Topics: Pulmonary Hypertension. National Heart, Lung and Blood Institute. National Library of Medicine. 24 March 2022.
- ^ a b c d "Treatment". Health Topics: Pulmonary Hypertension. National Heart, Lung and Blood Institute. National Library of Medicine. 24 March 2022.
- ^ a b c NHLBI & What Is Pulmonary Hypertension? 2023
- ^ "Diagnosis". Health Topics: Pulmonary Hypertension. National Heart, Lung and Blood Institute. National Library of Medicine. March 24, 2022.
- ^ von Romberg E (1891–1892). "Über Sklerose der Lungenarterie". Dtsch Arch Klin Med (in German). 48: 197–206.