| Rapidly progressive glomerulonephritis | |
|---|---|
| Other names | Crescentic glomerulonephritis[1] |
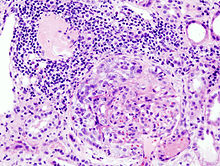 | |
| Histopathological image of crescentic glomerulonephritis in a patient with MPO-ANCA positive rapid progressive glomerulonephritis. Hematoxylin & eosin stain. | |
| Specialty | Nephrology |
| Symptoms | Hematuria[2] |
| Types | Type I, II and III[3] |
| Diagnostic method | Serum analysis[2] |
| Treatment | Corticosteroids |
Rapidly progressive glomerulonephritis (RPGN) is a syndrome of the kidney that is characterized by a rapid loss of kidney function,[4][5] (usually a 50% decline in the glomerular filtration rate (GFR) within 3 months)[5] with glomerular crescent formation seen in at least 50%[5] or 75%[4] of glomeruli seen on kidney biopsies. If left untreated, it rapidly progresses into acute kidney failure[6] and death within months. In 50% of cases, RPGN is associated with an underlying disease such as Goodpasture syndrome, systemic lupus erythematosus or granulomatosis with polyangiitis; the remaining cases are idiopathic. Regardless of the underlying cause, RPGN involves severe injury to the kidneys' glomeruli, with many of the glomeruli containing characteristic glomerular crescents (crescent-shaped scars).[7]
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Rapidly progressive glomerulonephritis". www.orpha.net. Retrieved 31 July 2019.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ a b Cite error: The named reference
robbinswas invoked but never defined (see the help page). - ^ Cite error: The named reference
isbn1-4200-8478-Xwas invoked but never defined (see the help page). - ^ a b TheFreeDictionary > rapidly progressive glomerulonephritis Citing: McGraw-Hill Concise Dictionary of Modern Medicine. 2002
- ^ a b c eMedicine > Glomerulonephritis, Crescentic Author: Malvinder S Parmar. Updated: Sep 25, 2008
- ^ "rapidly progressive glomerulonephritis" at Dorland's Medical Dictionary
- ^ Anguiano L, Kain R, Anders HJ (May 2020). "The glomerular crescent: triggers, evolution, resolution, and implications for therapy". Current Opinion in Nephrology and Hypertension. 29 (3): 302–309. doi:10.1097/MNH.0000000000000596. PMC 7170443. PMID 32132388.