| Rumination syndrome | |
|---|---|
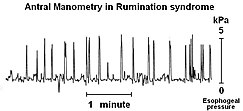 | |
| A postprandial manometry of a patient with rumination syndrome showing intra-abdominal pressure. The "spikes" are characteristic of the abdominal wall contractions responsible for the regurgitation in rumination. | |
| Specialty | Psychiatry |
Rumination syndrome, or merycism, is a chronic motility disorder characterized by effortless regurgitation of most meals following consumption, due to the involuntary contraction of the muscles around the abdomen.[1] There is no retching, nausea, heartburn, odour, or abdominal pain associated with the regurgitation as there is with typical vomiting, and the regurgitated food is undigested. The disorder has been historically documented as affecting only infants, young children, and people with cognitive disabilities (the prevalence is as high as 10% in institutionalized patients with various mental disabilities). It is increasingly being diagnosed in a greater number of otherwise healthy adolescents and adults, though there is a lack of awareness of the condition by doctors, patients, and the general public.
Rumination syndrome presents itself in a variety of ways, with especially high contrast existing between the presentation of the typical adult patient without a mental disability and the presentation of an adult with a mental disability. Like related gastrointestinal disorders, rumination can adversely affect normal functioning and the social lives of individuals. It has been linked with depression.
Little comprehensive data regarding rumination syndrome in otherwise healthy individuals exists because most people are private about their illness and are often misdiagnosed due to the number of symptoms and the clinical similarities between rumination syndrome and other disorders of the stomach and esophagus, such as gastroparesis and bulimia nervosa. These symptoms include the acid-induced erosion of the esophagus and enamel, halitosis, malnutrition, severe weight loss and an unquenchable appetite. Individuals may begin regurgitating within a minute following ingestion, and the full cycle of ingestion and regurgitation can mimic the binging and purging of bulimia.
Diagnosis of rumination syndrome is non-invasive and based on a history of the individual. Treatment is promising, with upwards of 85% of individuals responding positively to treatment, including infants and mentally disabled people.