| Scarlet fever | |
|---|---|
| Other names | Scarlatina,[1] scarletina[2] |
 | |
| White strawberry tongue in early stage | |
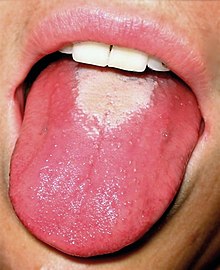 | |
| Red strawberry tongue seen in later stage | |
| Specialty | Infectious disease |
| Symptoms | Sore throat, fever, headaches, swollen lymph nodes in the neck, characteristic rash[1] |
| Complications | Kidney disease, rheumatic fever, arthritis[1] |
| Usual onset | 5–15 years old[1] |
| Causes | Group A streptococcal infection[3] |
| Diagnostic method | Throat culture[1] |
| Prevention | Handwashing, not sharing personal items, staying away from sick people[1] |
| Treatment | Antibiotics[1] |
| Medication | Penicillin VK, cefalexin, amoxicillin, clindamycin, erythromycin[4] |
| Prognosis | Typically good[1] |
Scarlet fever, also known as scarlatina, is an infectious disease caused by Streptococcus pyogenes, a Group A streptococcus (GAS).[3] It most commonly affects children between five and 15 years of age.[1] The signs and symptoms include a sore throat, fever, headache, swollen lymph nodes, and a characteristic rash.[1] The face is flushed and the rash is red and blanching.[5] It typically feels like sandpaper and the tongue may be red and bumpy.[1] The rash occurs as a result of capillary damage by exotoxins produced by S.pyogenes.[6] On darker-pigmented skin the rash may be hard to discern.[7]
Scarlet fever develops in a small number of people who have strep throat or streptococcal skin infections.[1] The bacteria are usually spread by people coughing or sneezing.[1] It can also be spread when a person touches an object that has the bacteria on it and then touches their mouth or nose.[1] The diagnosis is typically confirmed by culturing swabs of the throat.[1]
There is no vaccine for scarlet fever.[1] Prevention is by frequent handwashing, not sharing personal items, and staying away from other people when sick.[1] The disease is treatable with antibiotics, which reduce symptoms and spread, and prevent most complications.[1] Outcomes with scarlet fever are typically good if treated.[1] Long-term complications as a result of scarlet fever include kidney disease, rheumatic fever, and arthritis.[1]
In the early 20th century, scarlet fever was a leading cause of death in children, but even before World War II and the introduction of antibiotics, its severity was already declining. This decline is suggested to be due to better living conditions, the introduction of better control measures, or a decline in the virulence of the bacteria.[8][9] In recent years, there have been signs of antibiotic resistance; there was an outbreak in Hong Kong in 2011 and in the UK in 2014, and occurrence of the disease rose by 68% in the UK between 2014 and 2018. Research published in October 2020 showed that infection of the bacterium by three viruses has led to more virulent strains of the bacterium.[10]
- ^ a b c d e f g h i j k l m n o p q r s t "Scarlet Fever: All You Need to Know". Center for Disease Control and Prevention. 31 October 2022. Archived from the original on 15 December 2022. Retrieved 17 December 2022.
- ^ Shorter Oxford English dictionary. United Kingdom: Oxford University Press. 2007. p. 3804. ISBN 978-0199206872.
- ^ a b "Scarlet Fever: Information For Clinicians | CDC". www.cdc.gov. 19 December 2022. Archived from the original on 22 December 2022. Retrieved 22 December 2022.
- ^ Cite error: The named reference
Pardo2022was invoked but never defined (see the help page). - ^ Michaels, Marian `G.; Williams, John V. (2023). "13. Infectious diseases". In Zitelli, Basil J.; McIntire, Sara C.; Nowalk, Andrew J.; Garrison, Jessica (eds.). Zitelli and Davis' Atlas of Pediatric Physical Diagnosis (8th ed.). Philadelphia: Elsevier. pp. 468–471. ISBN 978-0-323-77788-9. Archived from the original on 8 April 2023. Retrieved 30 January 2023.
- ^ Stevens, Dennis L.; Bryant, Amy E. (2022). "21. Life-threatening skin and soft tissue infections". In Jong, Elaine C.; Stevens, Dennis L. (eds.). Netter's Infectious Diseases (2nd ed.). Elsevier. p. 95. ISBN 978-0-323-71159-3. Archived from the original on 22 April 2023. Retrieved 30 January 2023.
- ^ "Scarlet fever: symptoms, diagnosis and treatment". GOV.UK. Archived from the original on 11 December 2022. Retrieved 22 December 2022.
- ^ Smallman-Raynor, Matthew (2012). Atlas of epidemic Britain: a twentieth century picture. Oxford University Press. p. 48. ISBN 9780199572922. Archived from the original on 14 February 2017.
- ^ Welte, Alex; Williams, Brian; Hitchcock, Gavin (2017). "5.18. Mathematical models of transmission and control of infectious agents". In Detels, Roger; Gulliford, Martin; Karim, Quarraisha Abdool; Tan, Chorh Chuan (eds.). Oxford Textbook of Global Public Health. Vol. 1 (6th ed.). Oxford University Press. pp. 648–650. ISBN 978-0-19-871930-4. Archived from the original on 7 April 2023. Retrieved 30 January 2023.
- ^ Cite error: The named reference
abcviruswas invoked but never defined (see the help page).