| Sporotrichosis | |
|---|---|
| Other names | Rose thorn disease, rose gardener's disease,[1] rose handler's disease[2] |
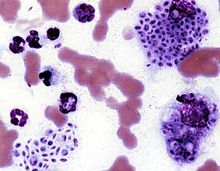 | |
| Cytologic preparation from a case of feline sporotrichosis; phagocytic cells show numerous variably-shaped yeast forms within | |
| Specialty | Infectious disease |
| Symptoms | Firm painless nodules that later ulcerate.[3] |
| Causes | Sporothrix schenckii[1] |
| Diagnostic method | |
| Differential diagnosis | Leishmaniasis, nocardiosis, mycobacterium marinum,[3] cat-scratch disease, syphilis, leprosy, sarcoidosis, tuberculosis[1] |
| Treatment | Antifungals, surgery[1] |
| Medication | Itraconazole, posaconazole, amphotericin B[1] |
| Prognosis | Good with treatment, poor if widespread disease[1] |
Sporotrichosis, also known as rose handler's disease,[2] is a fungal infection that may be localised to skin, lungs, bone and joint, or become systemic.[2][4] It presents with firm painless nodules that later ulcerate.[3] Following initial exposure to Sporothrix schenckii, the disease typically progresses over a period of a week to several months.[1] Serious complications may develop in people who have a weakened immune system.[1]
Sporotrichosis is caused by fungi of the S. schenckii species complex.[5][6] Because S. schenckii is naturally found in soil, hay, sphagnum moss, and plants, it most often affects farmers, gardeners, and agricultural workers.[7] It enters through small cuts in the skin to cause a fungal infection.[1] In cases of sporotrichosis affecting the lungs, the fungal spores enter by inhalation.[1] Sporotrichosis can be acquired by handling cats with the disease; it is an occupational hazard for veterinarians.[1]
Treatment depends on the site and extent of infection.[1] Topical antifungals may be applied to skin lesions.[1] Deep infection in the lungs may require surgery.[1] Systemic medications used include Itraconazole, posaconazole and amphotericin B.[1] With treatment, most people will recover,[1] but an immunocompromised status and systemic infection carry a worse prognosis.[1]
S. schenkii, the causal fungus, is found worldwide.[1] The species was named for Benjamin Schenck, a medical student who, in 1896, was the first to isolate it from a human specimen.[8]
Sporotrichosis has been reported in cats,[1] mules, dogs, mice and rats.[3]
- ^ a b c d e f g h i j k l m n o p q r s t u Milner, Dan A.; Solomon, Isaac (2020). "Sporotrichosis". In Milner, Danny A. (ed.). Diagnostic Pathology: Infectious Diseases. Elsevier. pp. 316–319. ISBN 978-0-323-61138-1.
- ^ a b c Proia, Laurie (2020). "28. The dimorphic mycoses". In Spec, Andrej; Escota, Gerome V.; Chrisler, Courtney; Davies, Bethany (eds.). Comprehensive Review of Infectious Diseases. Elsevier. pp. 421–422. ISBN 978-0-323-56866-1.
- ^ a b c d James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2019). "13. Diseases resulting from fungi and yeasts". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier. pp. 314–315. ISBN 978-0-323-54753-6.
- ^ Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 455. ISBN 978-0-7020-6830-0.
- ^ "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 11 July 2021.
- ^ López-Romero, Everardo; et al. (2010). "Sporothrix schenckii complex and sporotrichosis, an emerging health problem". Future Microbiology. 6 (1): 85–102. doi:10.2217/fmb.10.157. PMID 21162638.
- ^ Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 654–6. ISBN 978-0-8385-8529-0.
- ^ Barros MB, de Almeida Paes R, Schubach AO (October 2011). "Sporothrix schenckii and Sporotrichosis". Clinical Microbiology Reviews. 24 (4): 633–54. doi:10.1128/CMR.00007-11. PMC 3194828. PMID 21976602.