| Statin | |
|---|---|
| Drug class | |
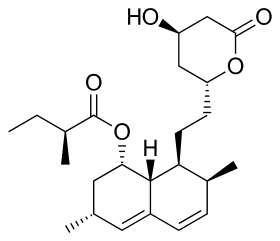 Lovastatin, a compound isolated from Aspergillus terreus, is the first statin to be marketed. | |
| Class identifiers | |
| Synonyms | HMG-CoA reductase inhibitors |
| Use | High cholesterol |
| ATC code | C10AA |
| Biological target | HMG-CoA reductase |
| Clinical data | |
| Drugs.com | Drug Classes |
| External links | |
| MeSH | D019161 |
| Legal status | |
| In Wikidata | |
Statins (or HMG-CoA reductase inhibitors) are a class of medications that reduce illness and mortality in people who are at high risk of cardiovascular disease.[1]
Low-density lipoprotein (LDL) carriers of cholesterol play a key role in the development of atherosclerosis and coronary heart disease via the mechanisms described by the lipid hypothesis. As lipid-lowering medications, statins are effective in lowering LDL cholesterol; they are widely used for primary prevention in people at high risk of cardiovascular disease, as well as in secondary prevention for those who have developed cardiovascular disease.[2][3][4]
Side effects of statins include muscle pain, increased risk of diabetes, and abnormal blood levels of certain liver enzymes.[5] Additionally, they have rare but severe adverse effects, particularly muscle damage, and very rarely rhabdomyolysis.[6][7]
They act by inhibiting the enzyme HMG-CoA reductase, which plays a central role in the production of cholesterol. High cholesterol levels have been associated with cardiovascular disease.[8]
There are various forms of statins, some of which include atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin.[9] Combination preparations of a statin and another agent, such as ezetimibe/simvastatin, are also available. The class is on the World Health Organization's List of Essential Medicines with simvastatin being the listed medicine.[10] In 2005, sales were estimated at US$18.7 billion in the United States.[11] The best-selling statin is atorvastatin, also known as Lipitor, which in 2003 became the best-selling pharmaceutical in history.[12] The manufacturer Pfizer reported sales of US$12.4 billion in 2008.[13]
Patient compliance with statin usage is problematic despite robust evidence of the benefits.[14][15]
- ^ "Cholesterol Drugs". American Heart Association. Archived from the original on 12 August 2020. Retrieved 24 December 2019.
- ^ Alenghat FJ, Davis AM (February 2019). "Management of Blood Cholesterol". JAMA. 321 (8): 800–801. doi:10.1001/jama.2019.0015. PMC 6679800. PMID 30715135.
- ^ National Clinical Guideline Centre (UK) (July 2014). Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. National Institute for Health and Clinical Excellence: Guidance. London: National Institute for Health and Care Excellence (UK). PMID 25340243. NICE Clinical Guidelines, No. 181. Archived from the original on 29 May 2020. Retrieved 26 April 2020 – via National Library of Medicine.
- ^ Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. (January 2013). "Statins for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2013 (1): CD004816. doi:10.1002/14651858.CD004816.pub5. PMC 6481400. PMID 23440795.
- ^ Naci H, Brugts J, Ades T (July 2013). "Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials". Circulation: Cardiovascular Quality and Outcomes. 6 (4): 390–399. doi:10.1161/CIRCOUTCOMES.111.000071. PMID 23838105. S2CID 18340552.
- ^ Abd TT, Jacobson TA (May 2011). "Statin-induced myopathy: a review and update". Expert Opinion on Drug Safety. 10 (3): 373–387. doi:10.1517/14740338.2011.540568. PMID 21342078. S2CID 207487287.
- ^ "Should you be worried about severe muscle pain from statins?". Mayo Clinic. Archived from the original on 15 May 2024. Retrieved 30 October 2023.
- ^ Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, et al. (December 2007). "Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths". The Lancet. 370 (9602): 1829–1839. doi:10.1016/S0140-6736(07)61778-4. PMID 18061058. S2CID 54293528.
- ^ Sweetman SC, ed. (2009). "Cardiovascular drugs". Martindale: The Complete Drug Reference (36th ed.). London: Pharmaceutical Press. pp. 1155–1434. ISBN 978-0-85369-840-1.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Taylor FC, Huffman M, Ebrahim S (December 2013). "Statin therapy for primary prevention of cardiovascular disease". JAMA. 310 (22): 2451–2452. doi:10.1001/jama.2013.281348. PMID 24276813.
- ^ Cite error: The named reference
Simonswas invoked but never defined (see the help page). - ^ "2008 Annual Report" (PDF). Pfizer. 23 April 2009. p. 15. Archived (PDF) from the original on 12 May 2013.
- ^ Maningat P, Gordon BR, Breslow JL (January 2013). "How do we improve patient compliance and adherence to long-term statin therapy?". Current Atherosclerosis Reports. 15 (1): 291. doi:10.1007/s11883-012-0291-7. PMC 3534845. PMID 23225173.
- ^ Tarn D, Pletcher M, Tosqui R (June 2021). "Primary nonadherence to statin medications: Survey of patient perspectives". Preventive Medicine Reports. 22: 101357. doi:10.1016/j.pmedr.2021.101357. PMC 8020471. PMID 33842201.